Alke was a final project for my master’s degree in Service Design from the Royal College of Art.
My project partner and I had personal experiences with relatives suffering from a brain tumour. As a result, we acknowledged the need for improvement in the whole experience. In close collaboration with brain tumour survivors, their relatives, as well as experts in the field, we developed a support service leveraging technology for patients and carers.
Project Alke was also a finalist for the Service Design Award 2018, an international award for service design, as well as finalist for the Helen Hamlyn Centre for Design, an RCA award where entrants are nominated by Royal College of Art professors and heads of department.
Bus Open Data
Making data open and available
Alke is a service for people with a brain tumour and their carers, that helps them understand, adapt and easily manage their rehabilitation on a daily basis.
Alke facilitates the rehabilitation experience of patients with a brain tumour and their carers by:
Enhancing self-management.
Introducing a digital communication channel for patients and their carers to connect with clinicians.
Providing a holistic and personalised approach that understands the patient’s status.
Supporting them in strengthening their cognitive and physical functions through engaging activities.
The overall aim of the service is to enable patients to be in charge of their rehabilitation journey. Alke has 3 main components that play together in one holistic journey: the App, the Box and the Bracelet. These three components along with a back-end of data analysis, kit personalisation, and technical & customer support, align with the established objectives and improve the rehabilitation experience for both patients and carers.
Introduction
In the UK, there are more than 11,500 new cases of brain tumours every year, which is equal to a 34% increase in the incidence rate of brain tumours since the 90s. At least 102,000 children and adults are currently living with a brain tumour in the UK alone.
According to the Commissioning Guidance for Rehabilitation, the aim of the NHS is to do more than just stop people dying but to equip them to live their lives, fulfil their maximum potential, and optimise their contribution to family life.
When we started this project, we shared the same goal.
To further understand the core of the problem, we travelled around England and met with patients and carers.
The people we talked to included survivors, terminal patients, and carers.
In parallel, we also ran online surveys and plenty of desk research, as well as expert interviews with a rehabilitation consultant, a foundation doctor, the Head of Support for a support charity, and an entrepreneur in Digital Health innovation.
We analysed the findings into 4 main categories:
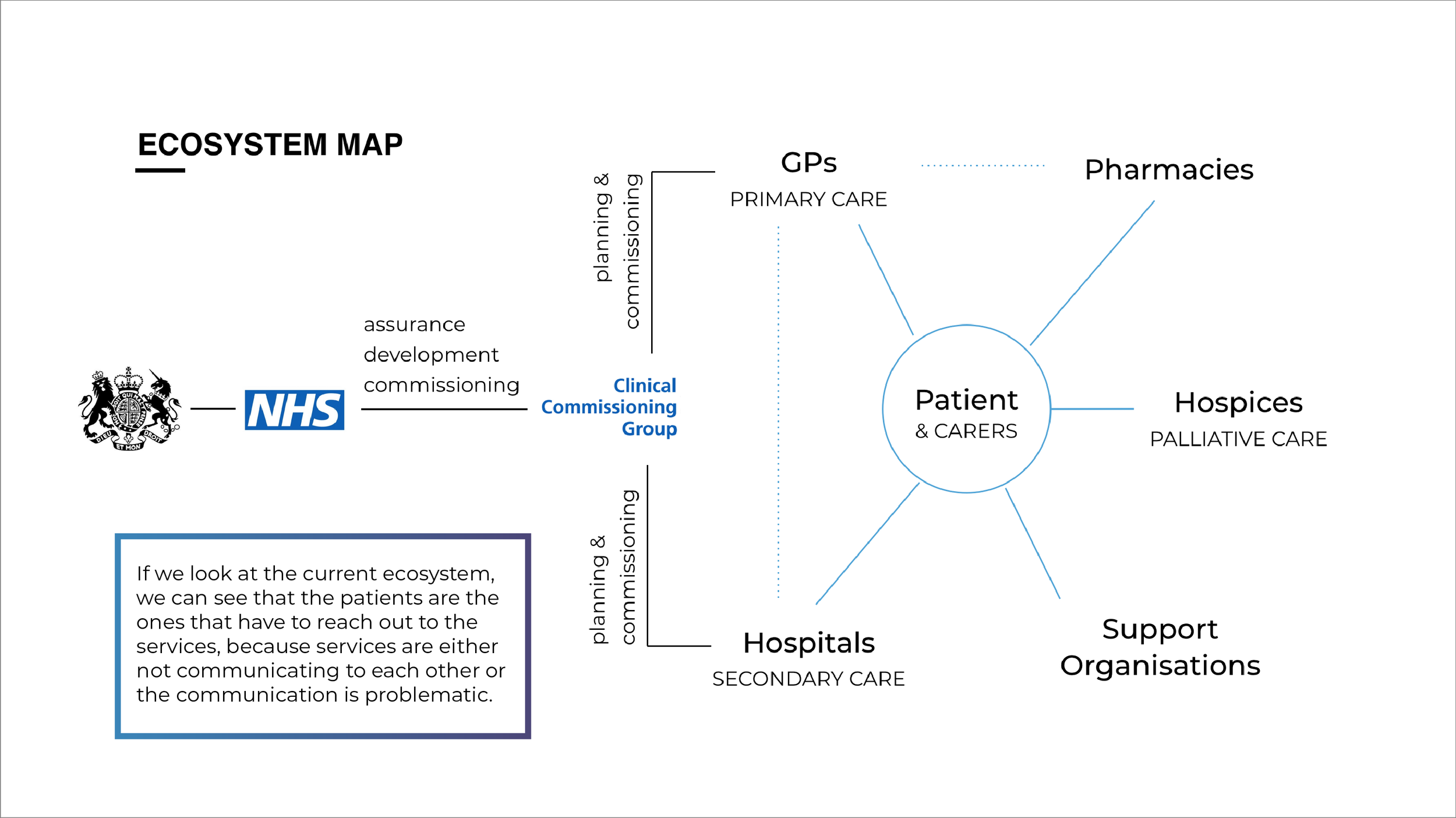
Healthcare System
Business Case
Technology
User Experience
Our findings are as follows:
Current Experience
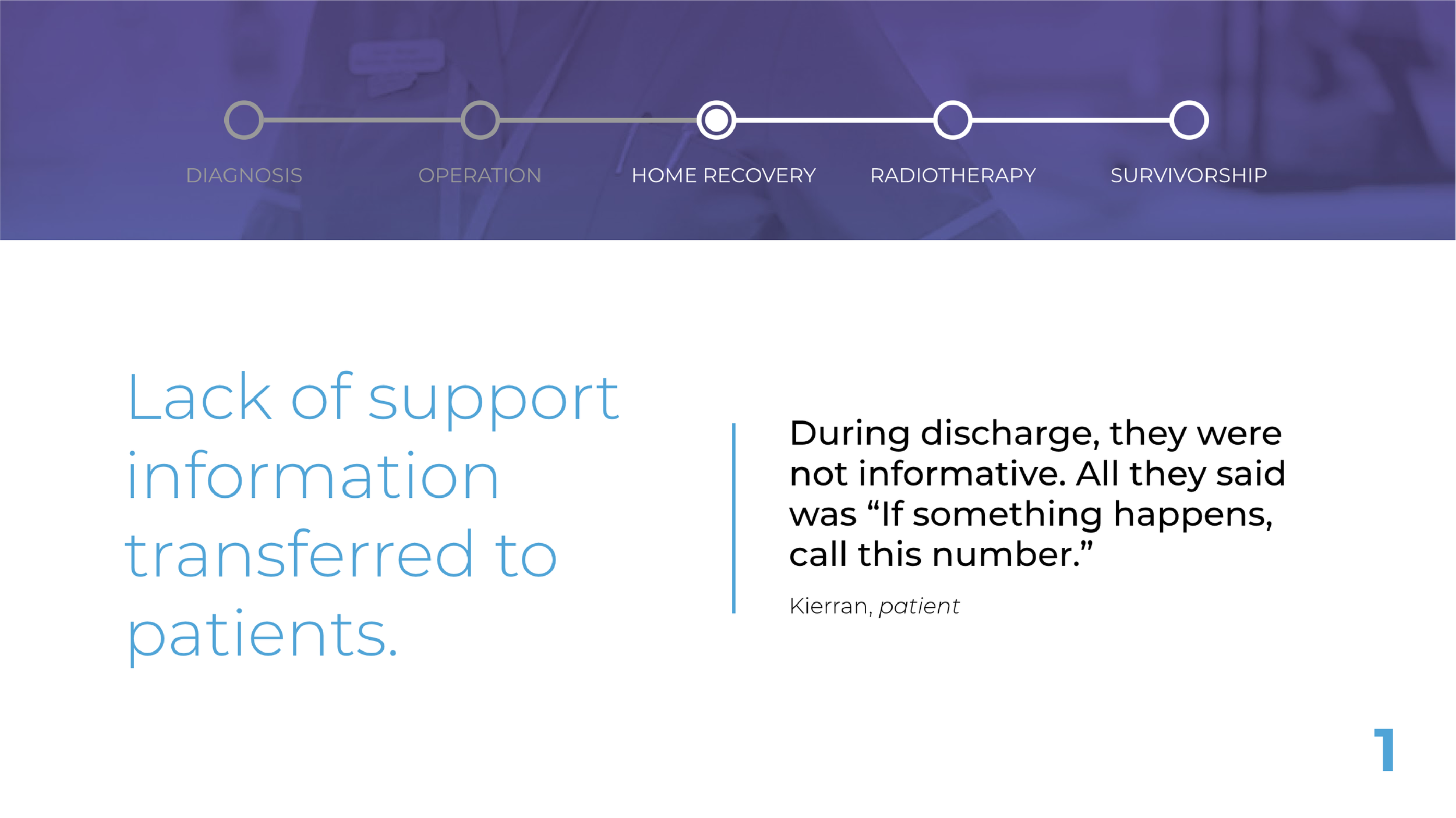
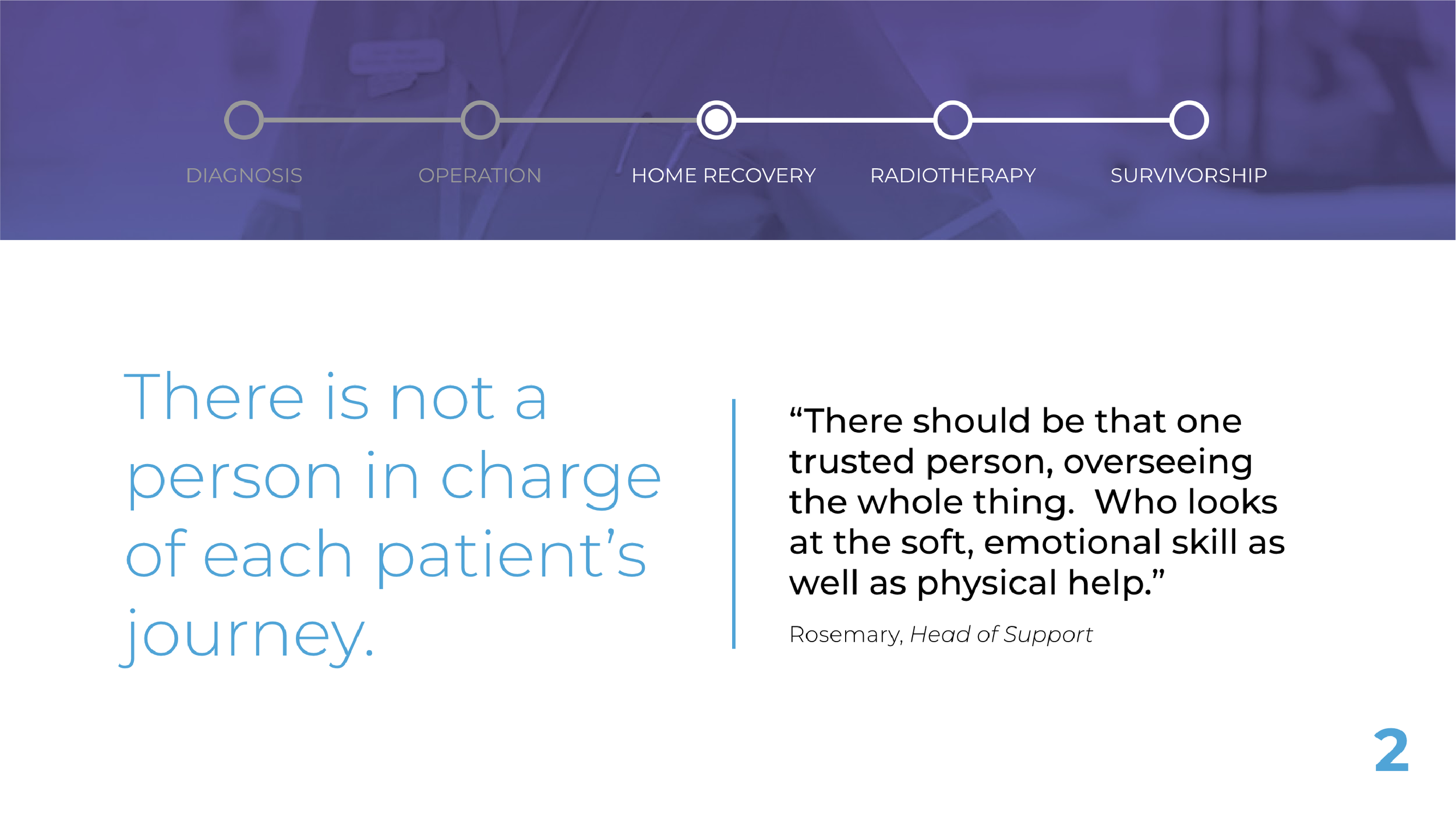
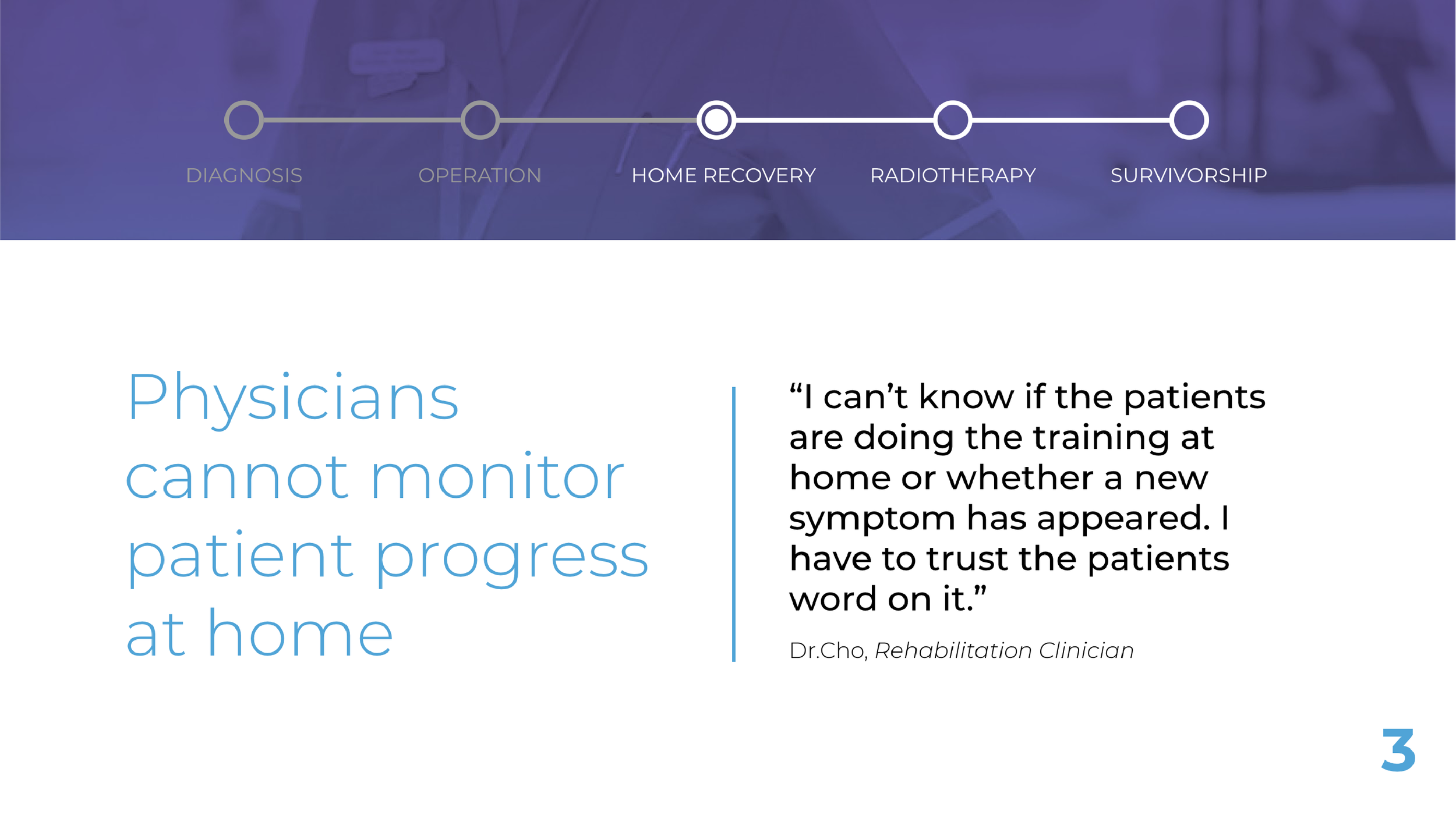
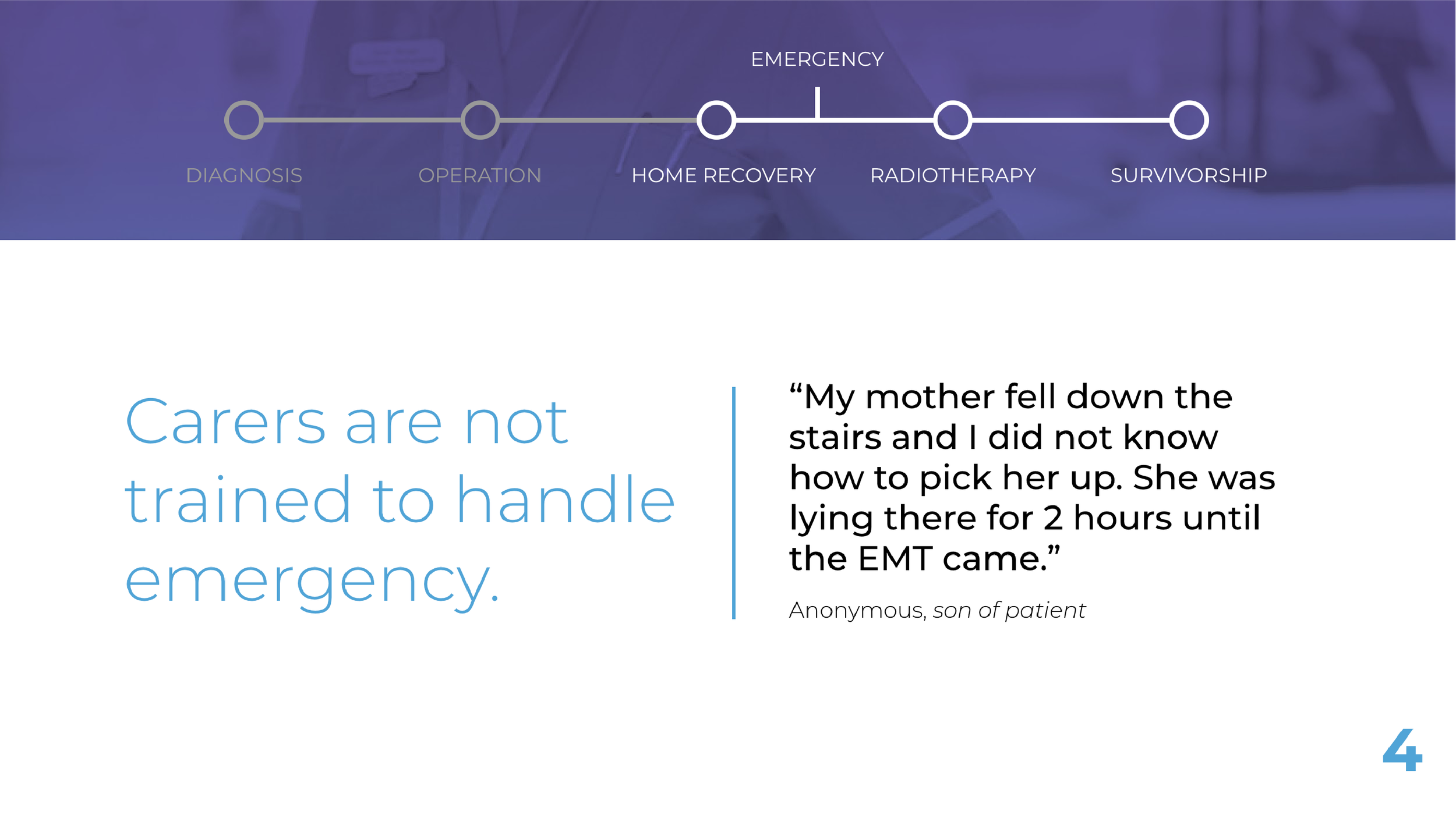
From a high-level, they usually go through a 5-step journey: from Diagnosis, one or more possible Operations, Home Recovery and multiple Radiotherapy sessions to Survivorship. However, as mentioned in our findings, every brain tumour case is different and can vary greatly, and therefore we cannot put people’s journey in boxes.
Our focus is on the last bit, the rehabilitation experience.
Let’s briefly look at some of the pains which patients and carers face during this phase.
We could identify different stages within the emotional journey of patients during the rehabilitation experience.
With all the insights, we identified 6 variables:
Control: Patients and carers feel like they’re losing control and that the tumour is driving their lives.
Communication: Communication between patients and carers, as well as with clinicians, is difficult and inefficient.
Trust: Patients and carers do not fully trust the clinicians and the system.
Convenience: Patients need a simple, concise and easy way to access service.
Dignity: Patients are losing confidence and dignity through their battle with the tumour .
Emotion: Patients and carers go through an emotional roller-coaster during the journey due to a lack of support and information.
Problem Statement
These variables helped us shape our problem statement for our two main stakeholders:
Alke
Alke (from the spirit of courage in Greek mythology) is a service for people with a brain tumour and their carers, which helps them understand, adapt and easily manage their rehabilitation on a daily basis.
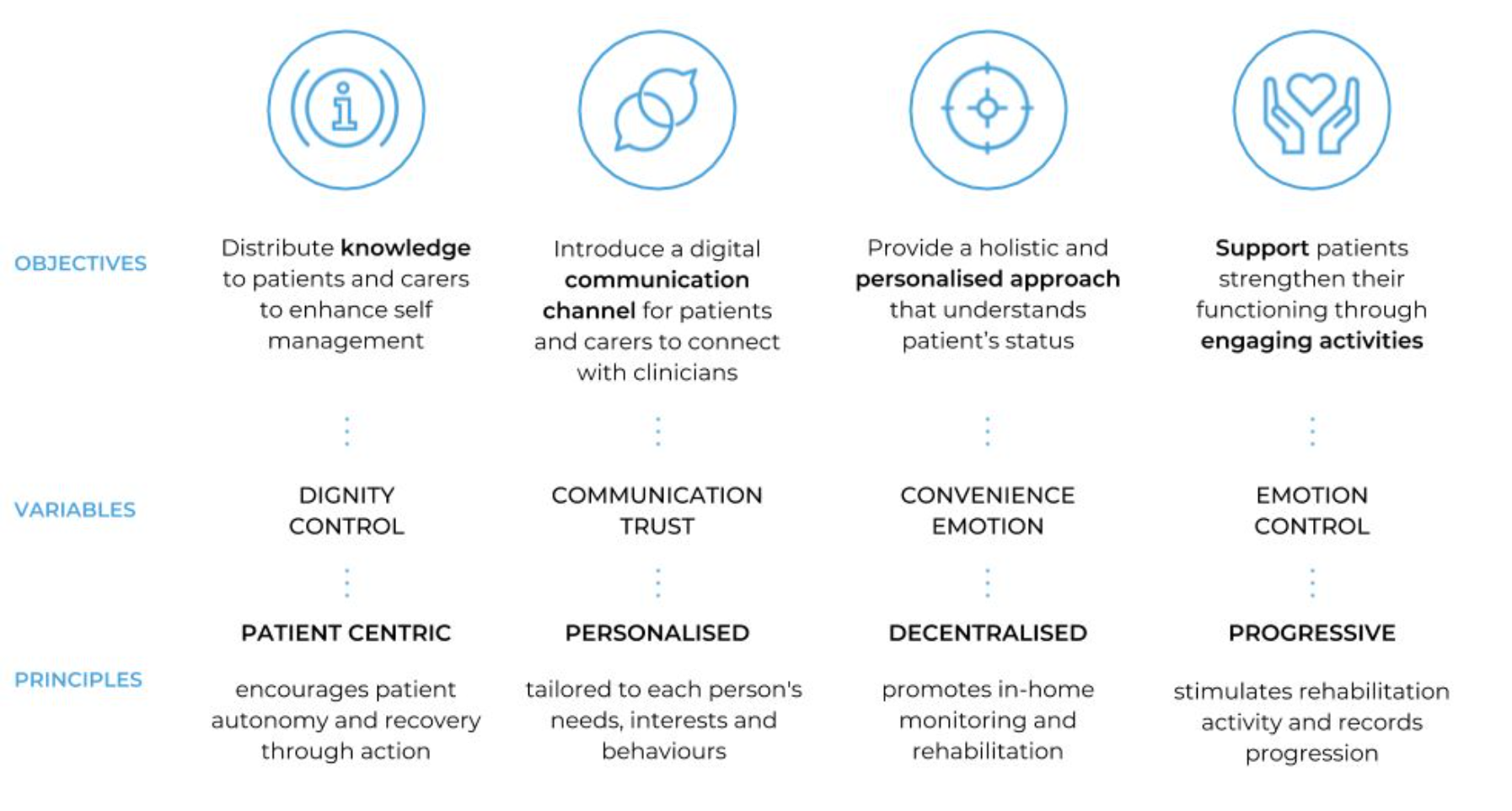
The 4 main objectives of Alke align with the variables it’s designed to focus on:
These reflect our principles; to be patient centric, personalised, decentralised and progressive.
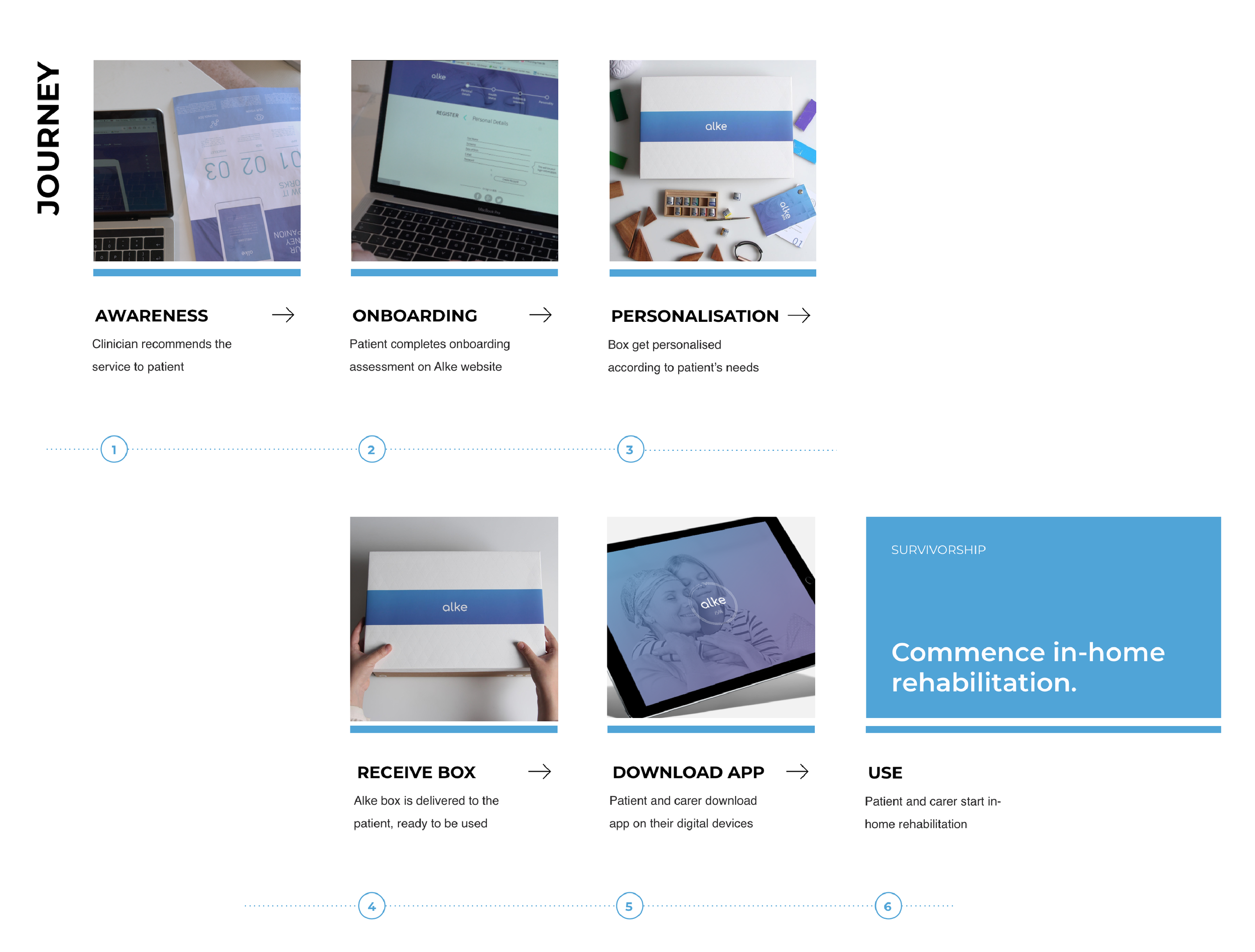
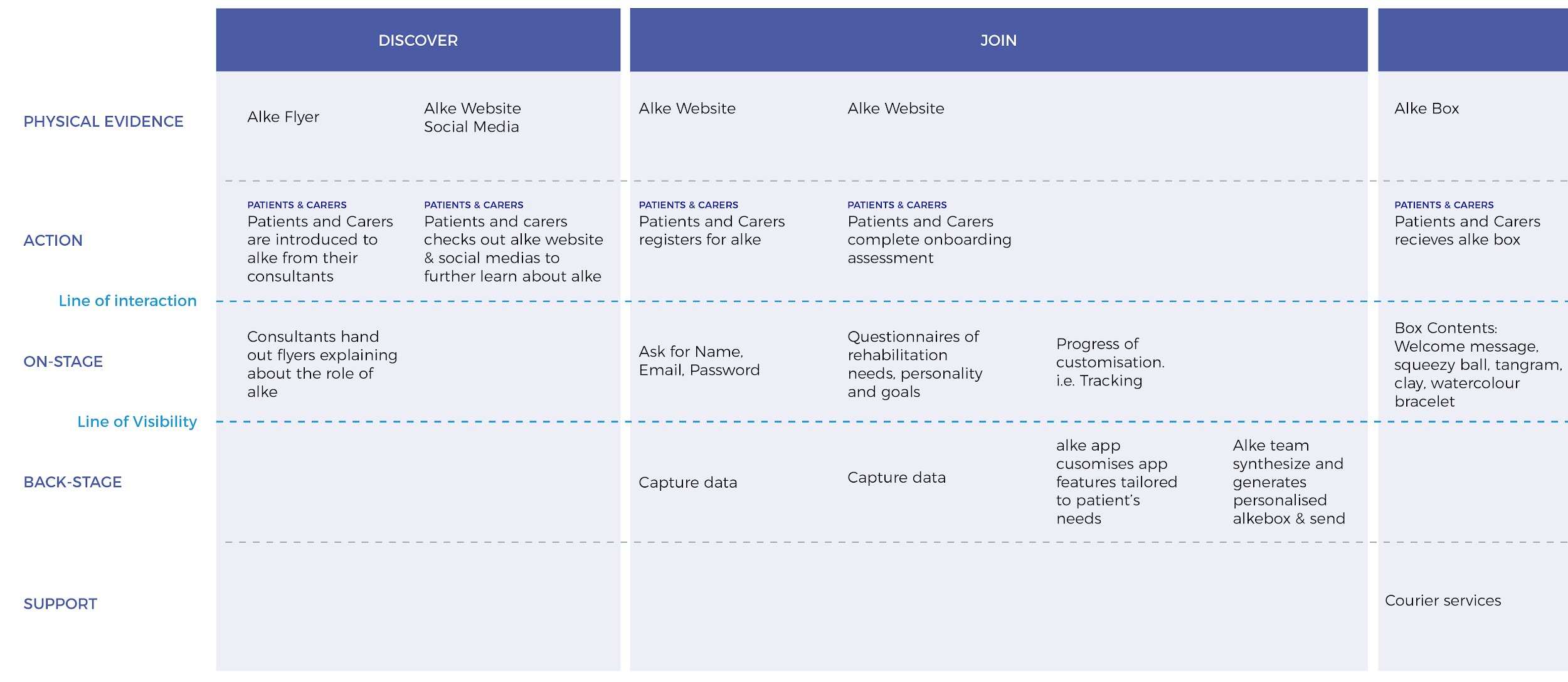
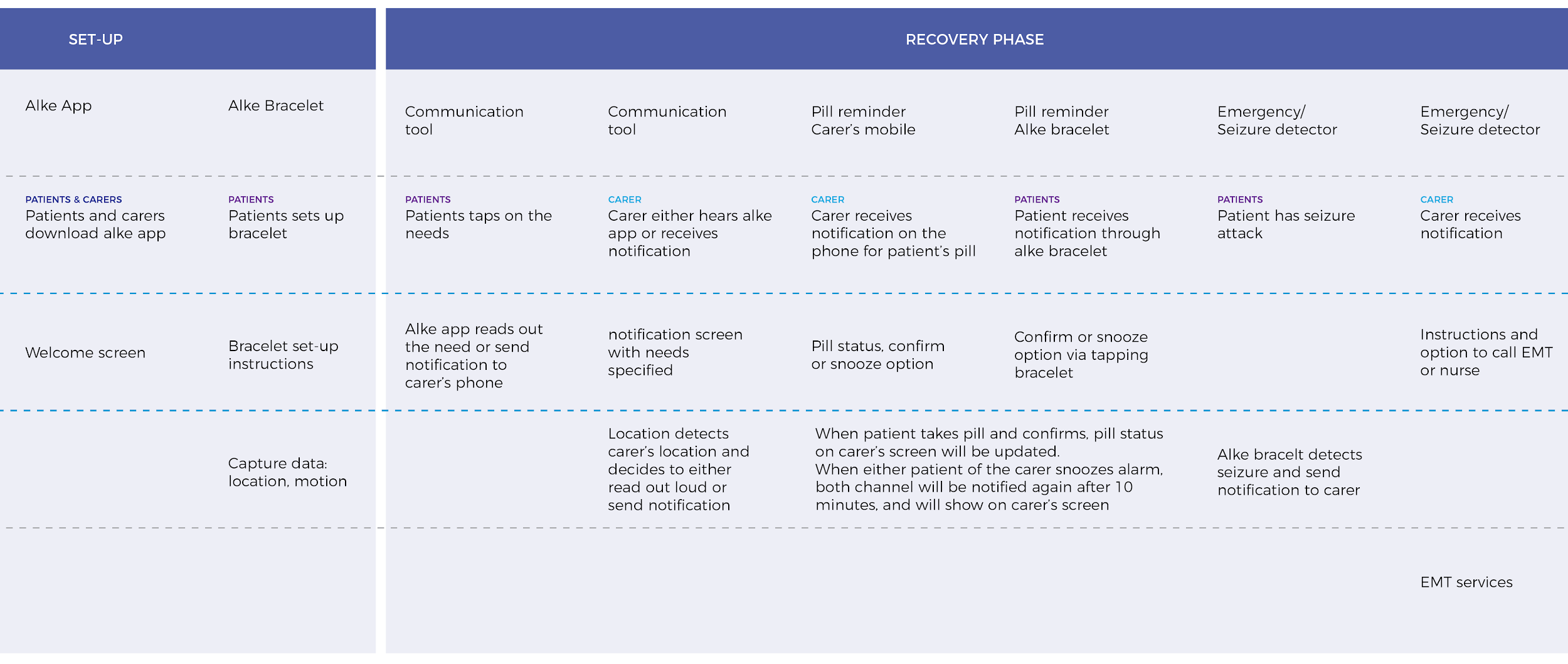
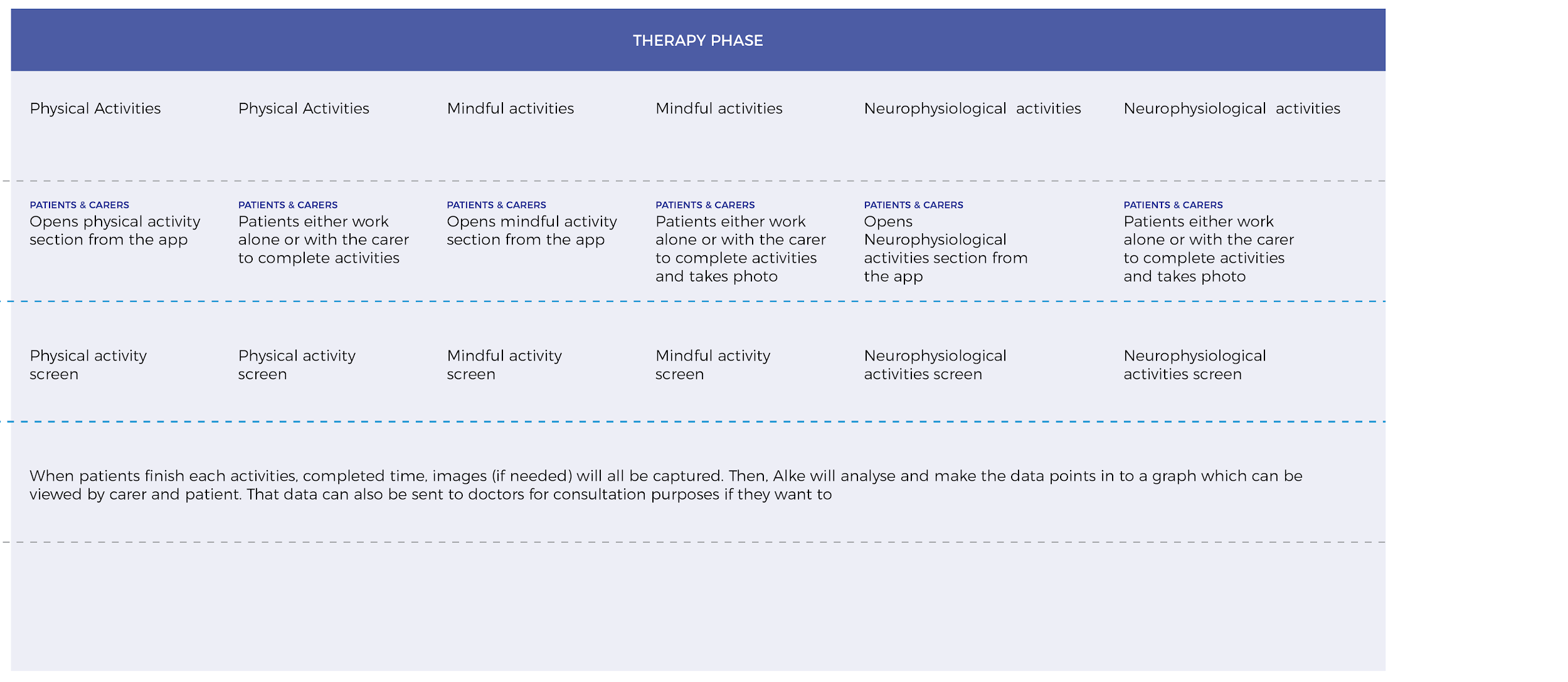
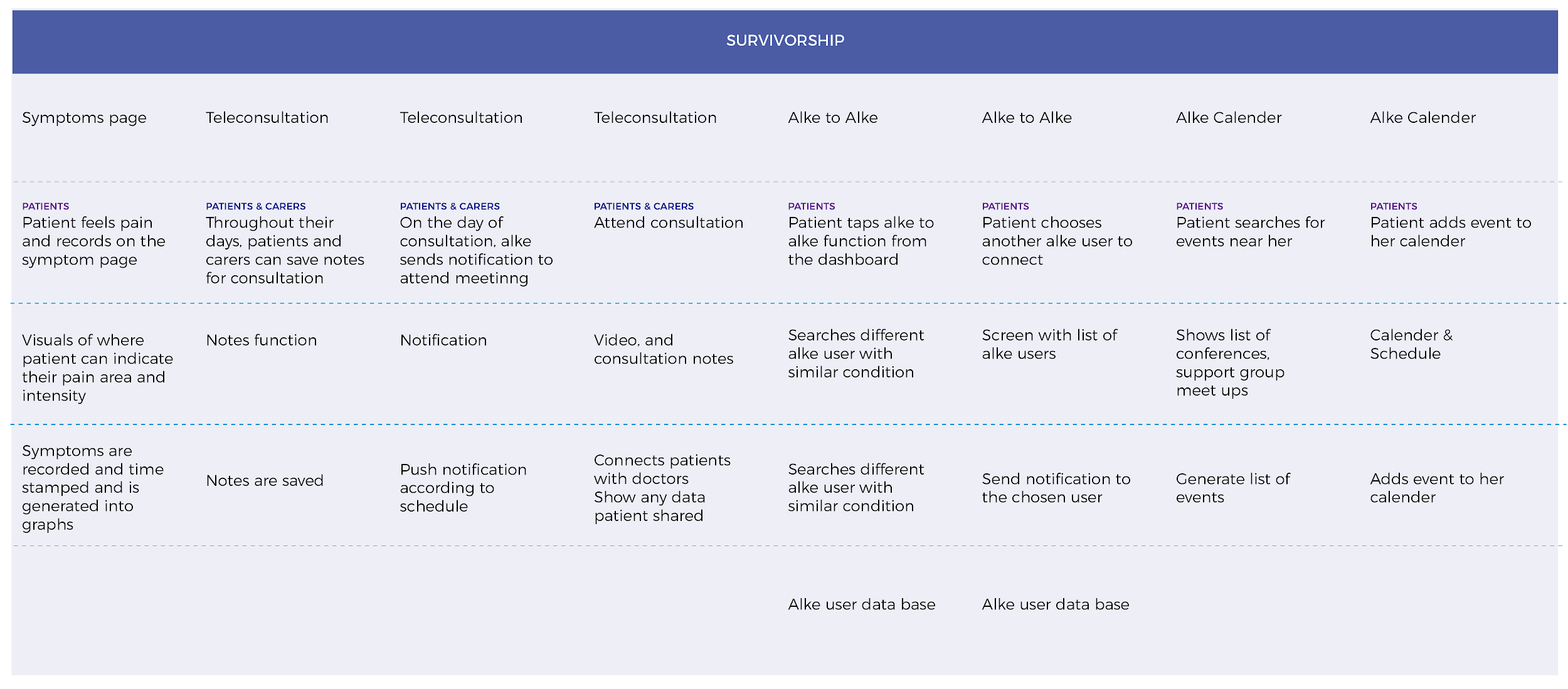
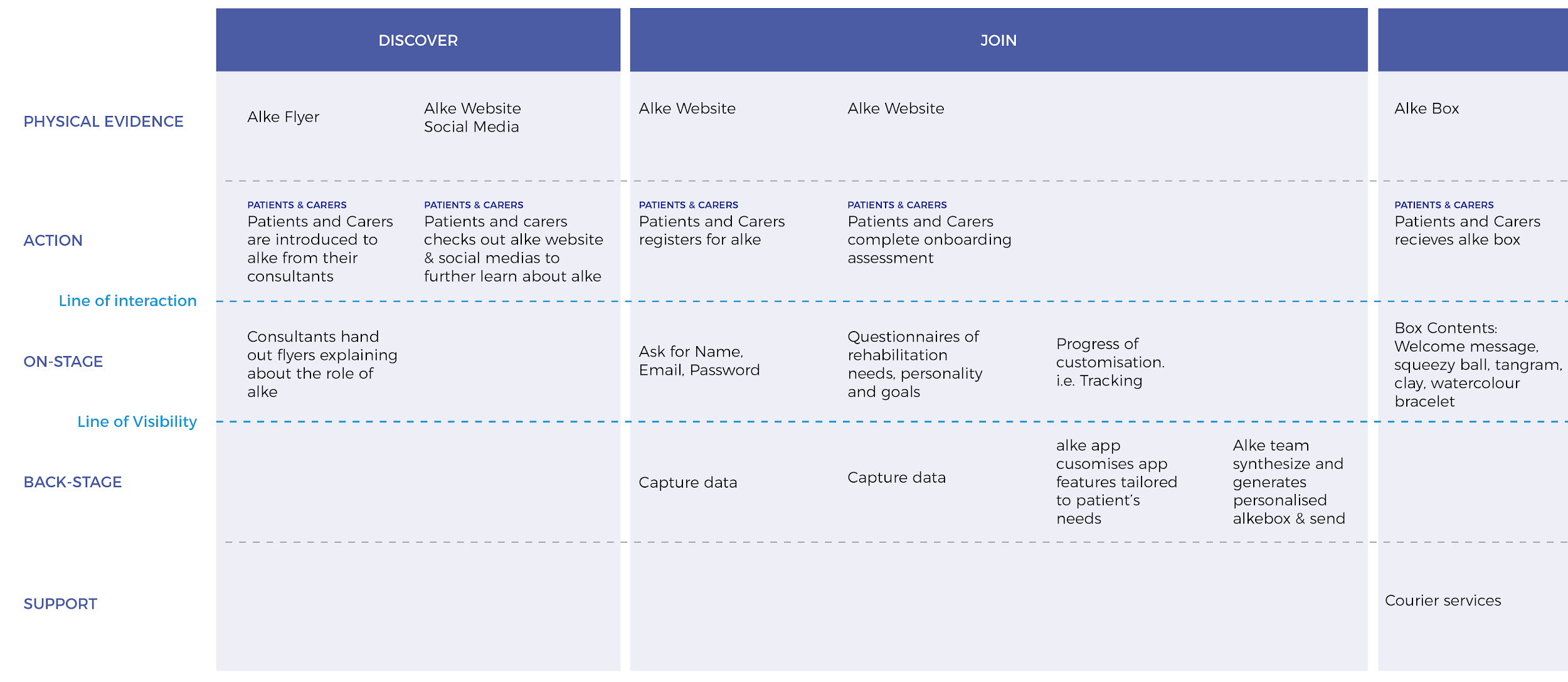
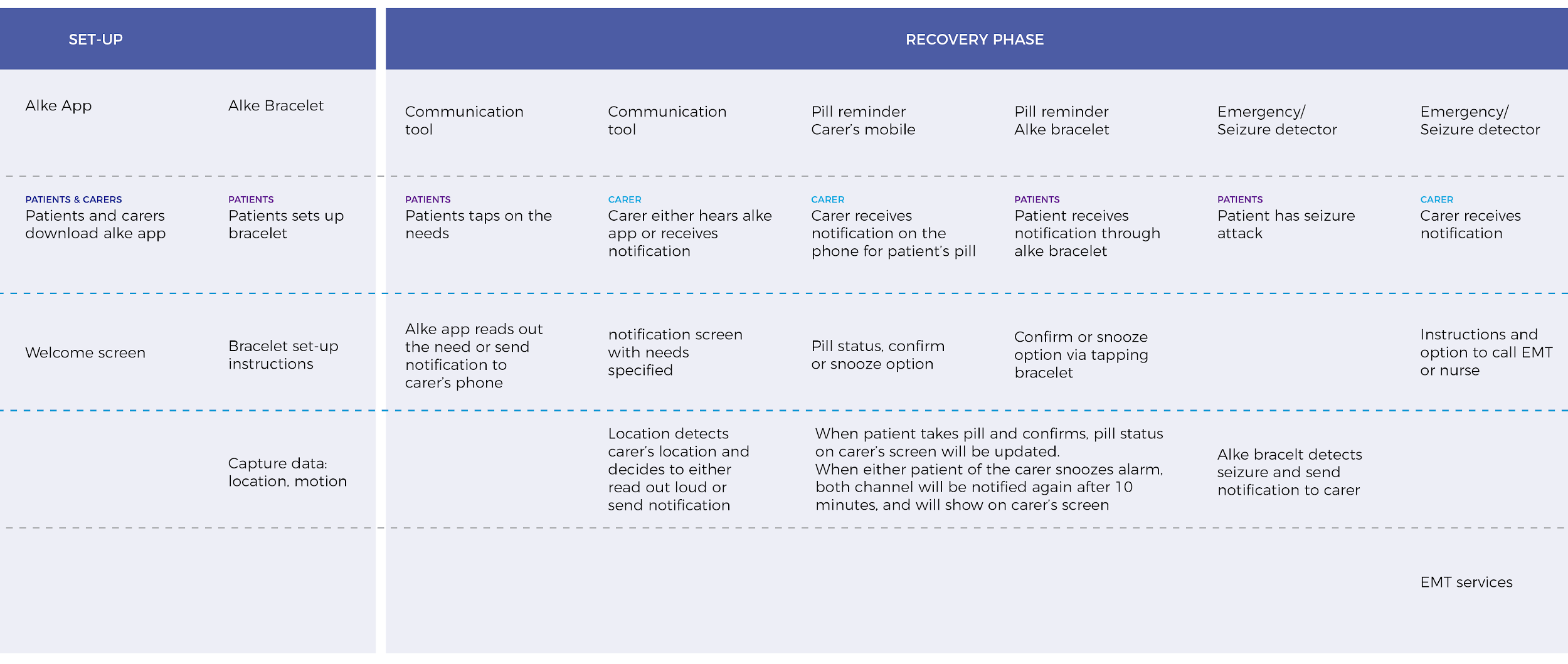
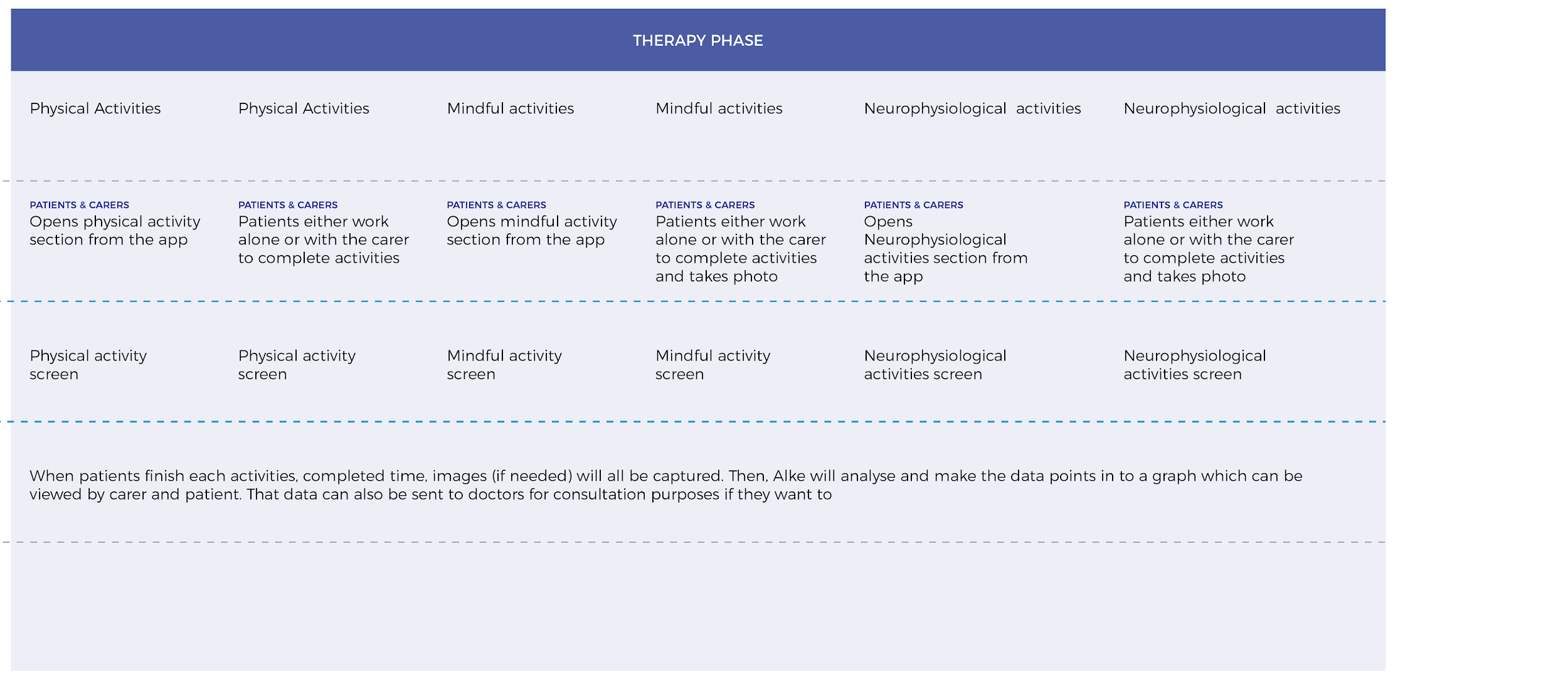
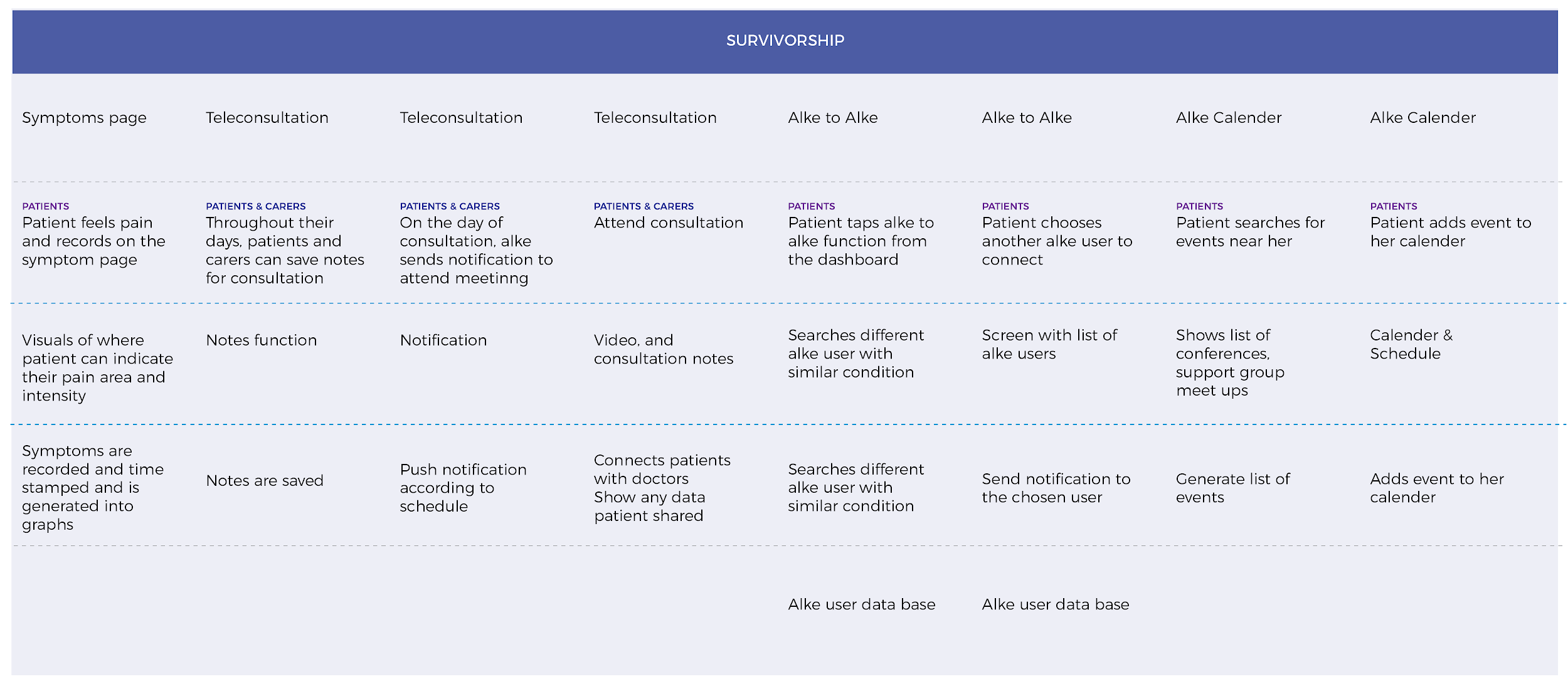
The service blueprint for Alke:
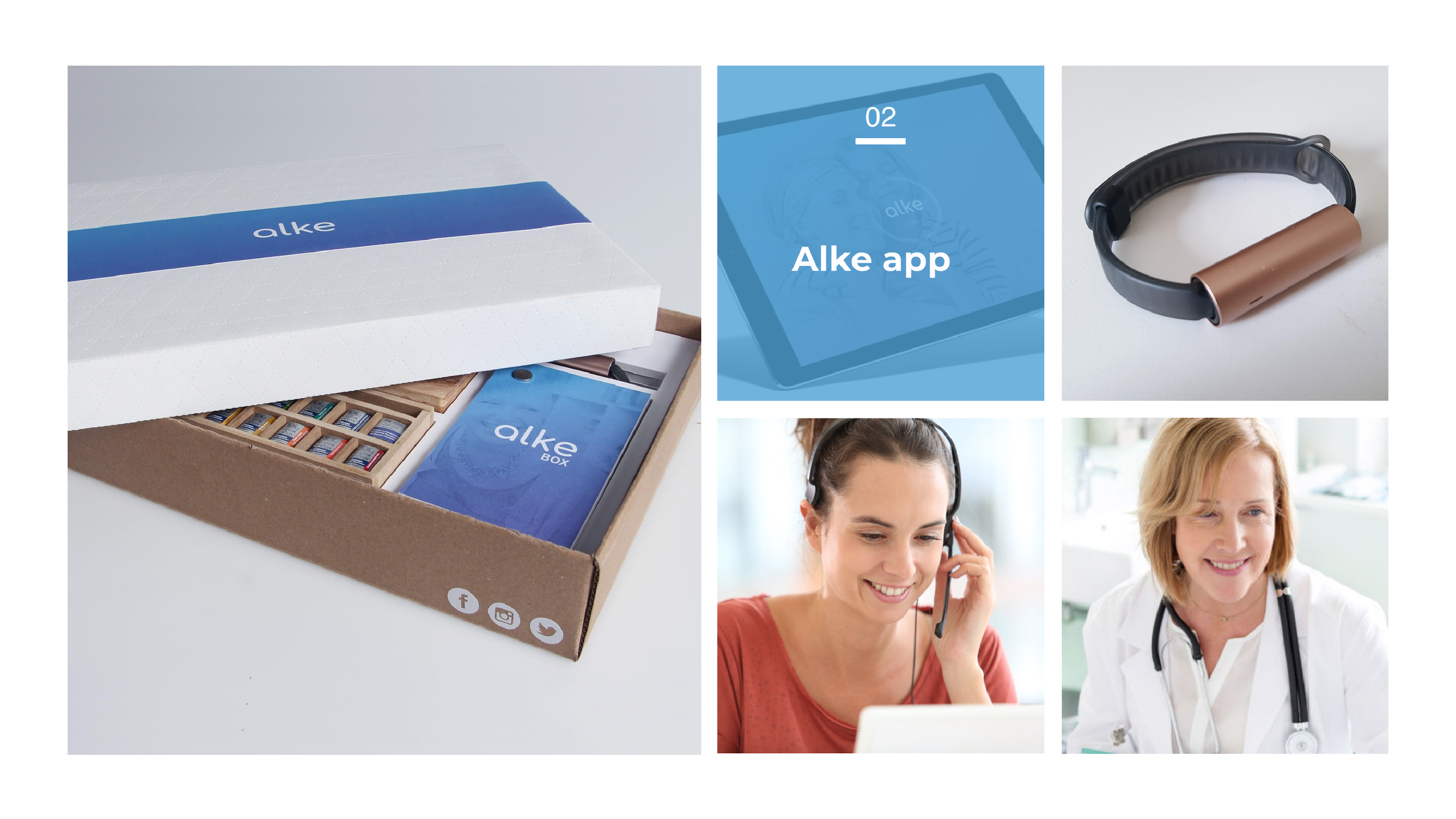
Alke’s Components
Alke is composed with 5 different components:
Alke Box
Alke App
Alke Bracelet
Back-end
Support
Alke Box — A personalised kit for patients, which includes the necessary props for their rehabilitation; its contents are customised depending on the patient’s needs and interests.
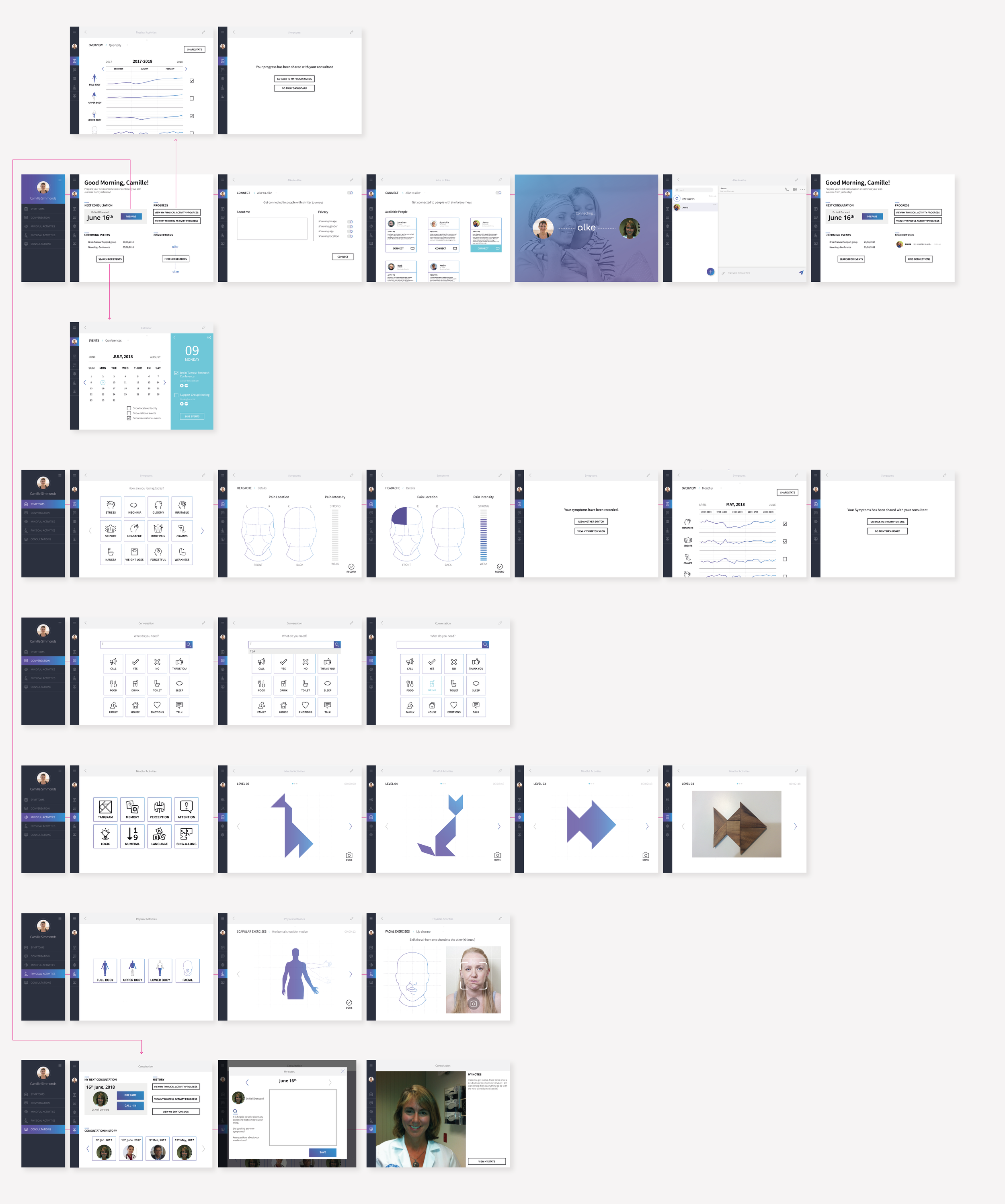
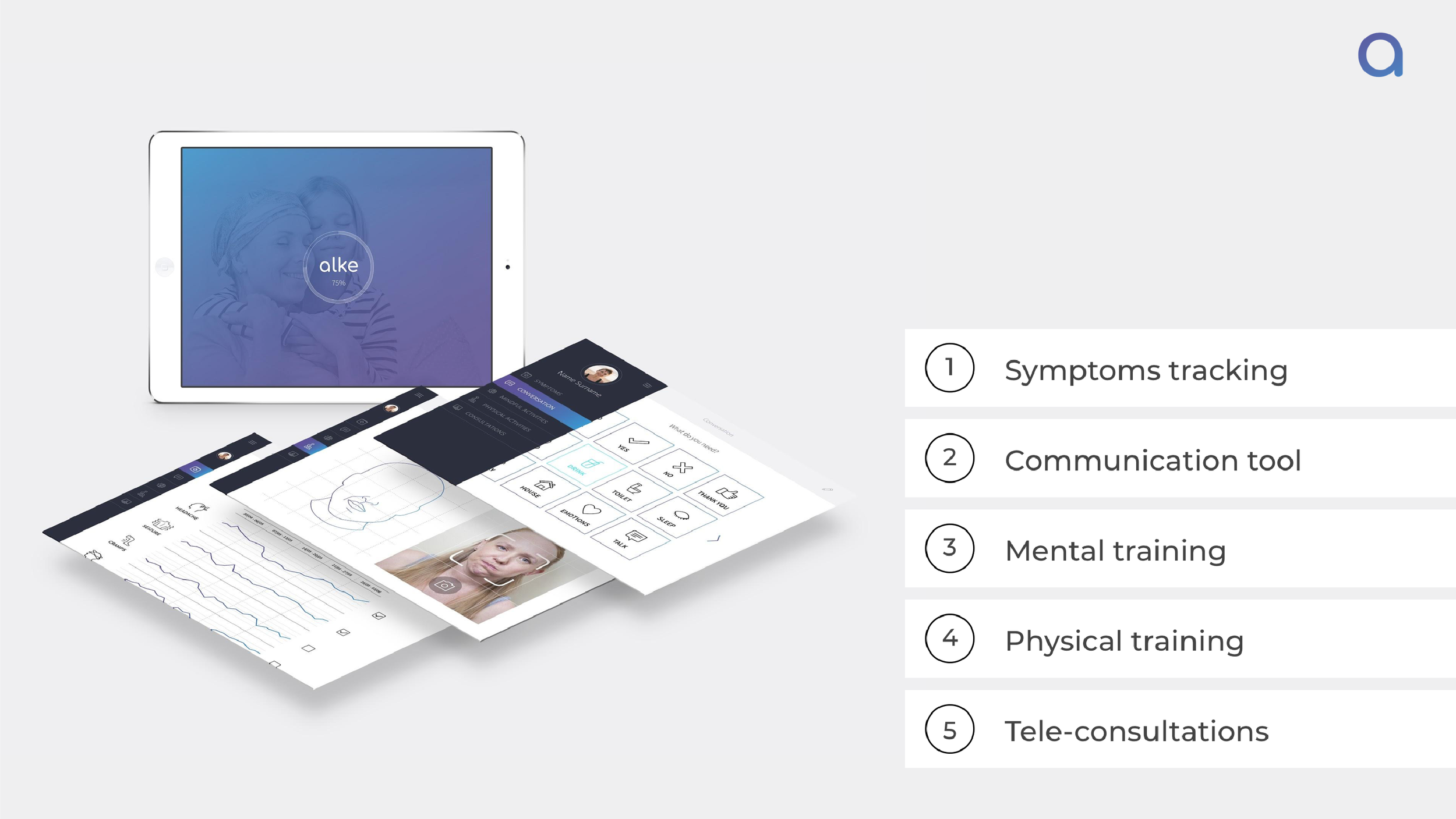
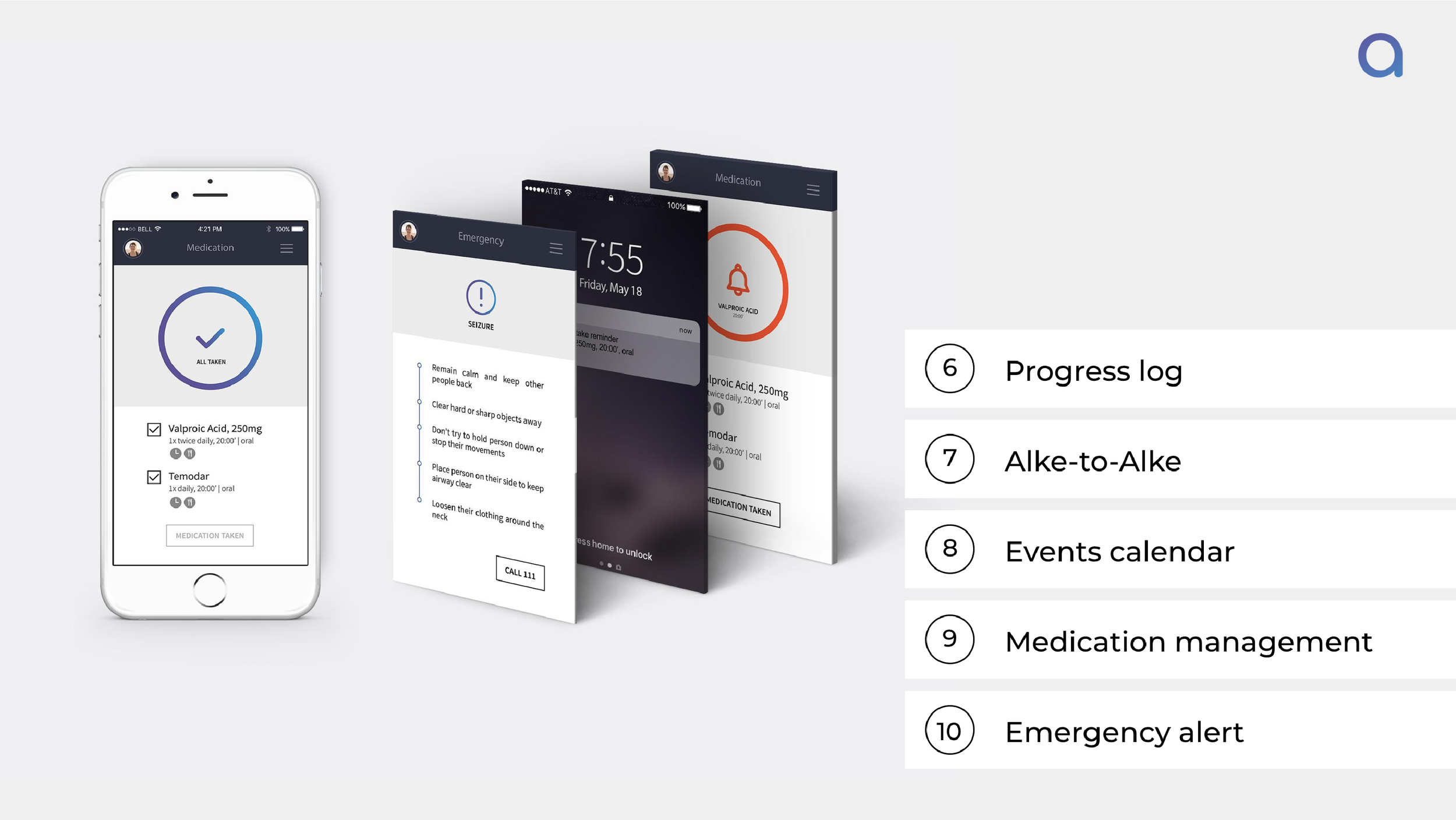
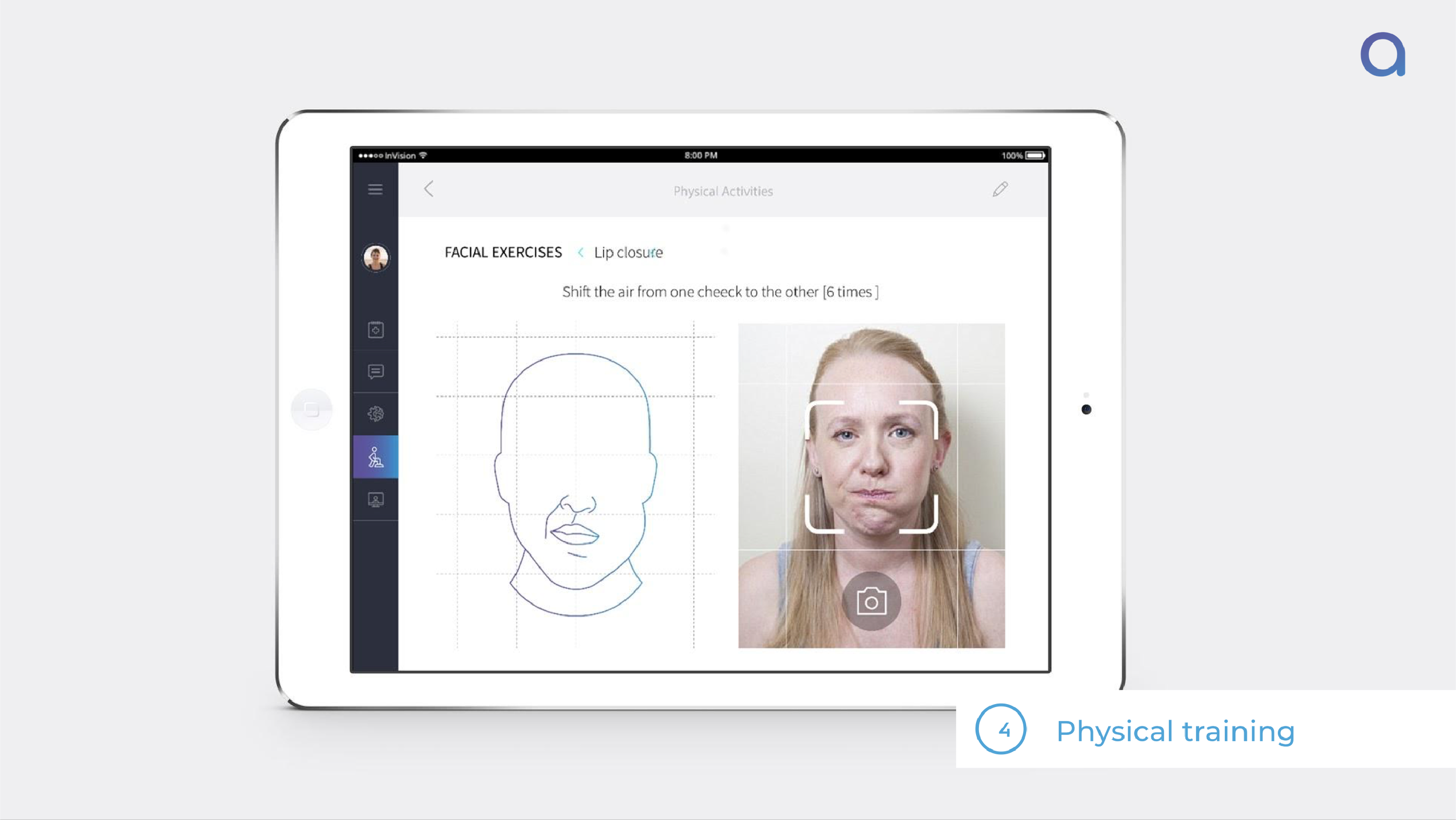
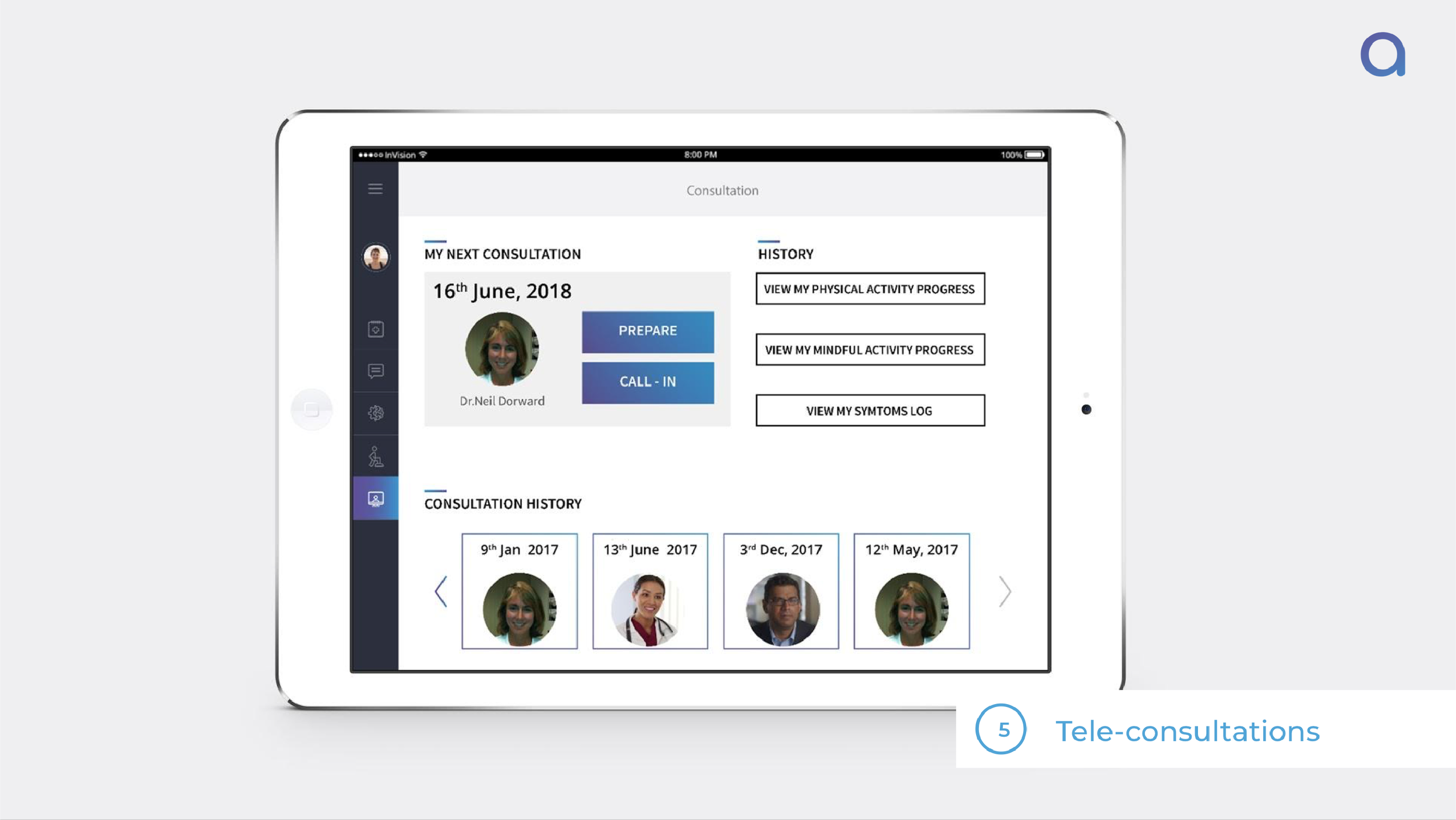
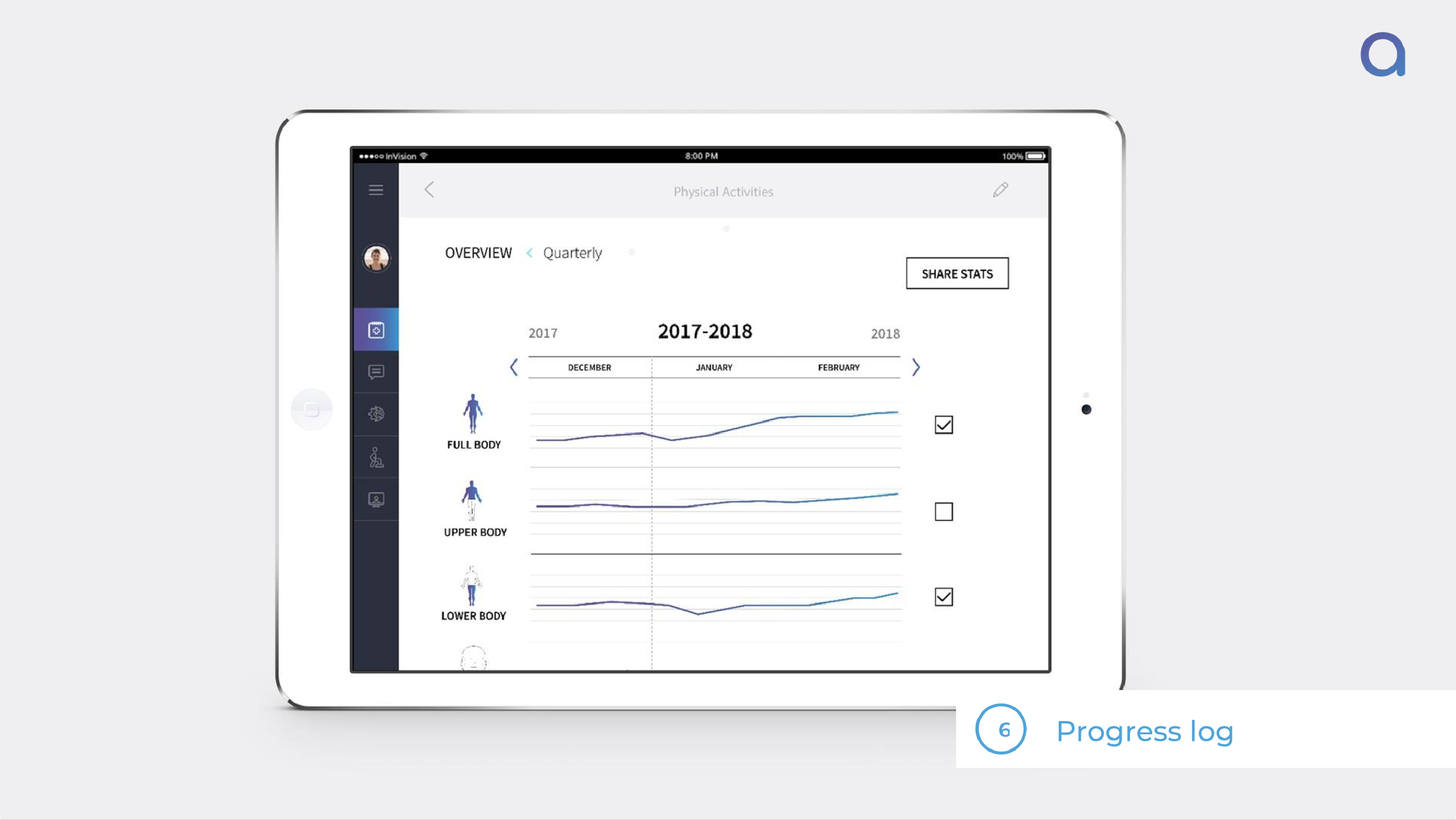
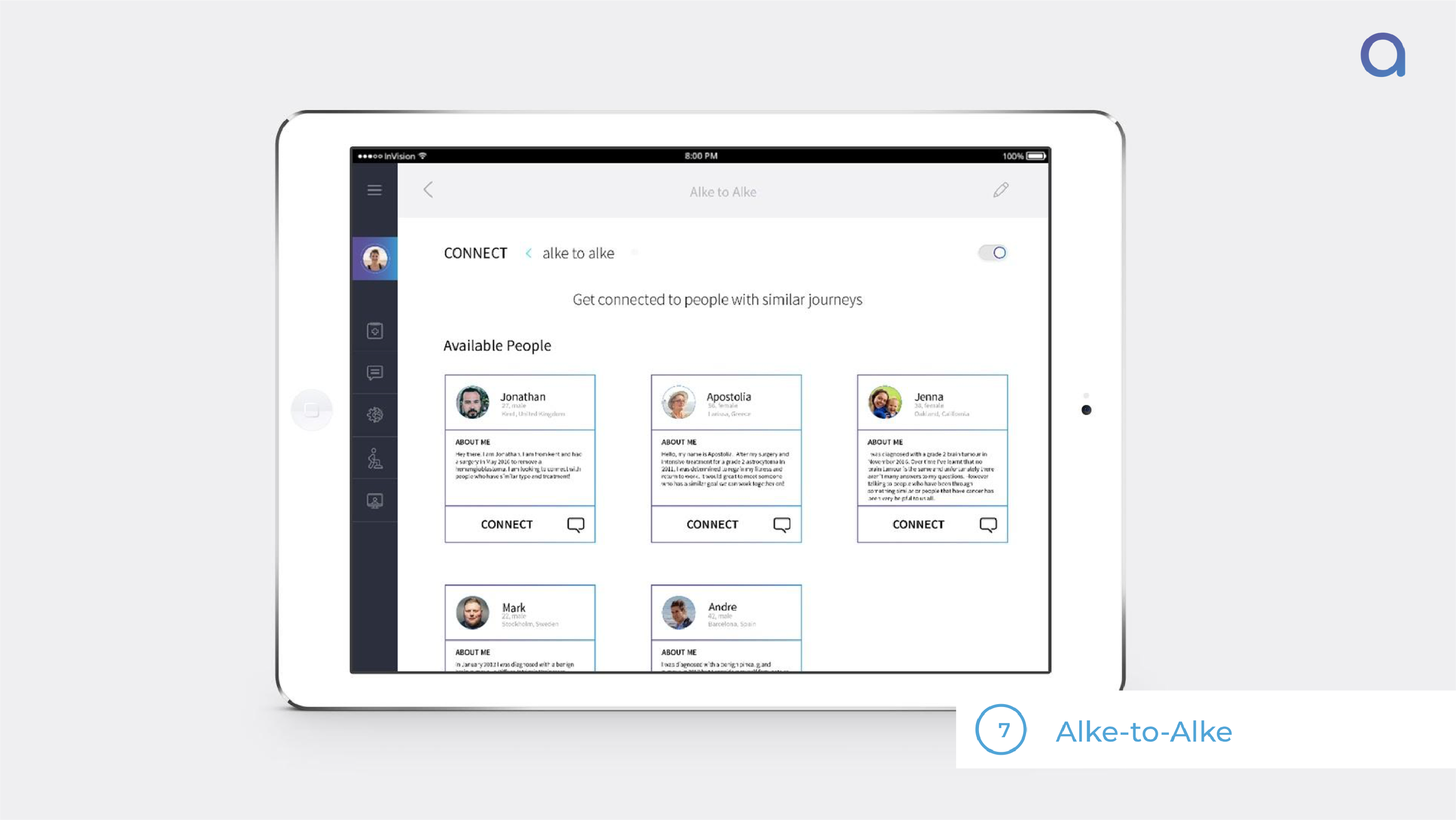
Alke App — An app promoting self-monitoring, rehabilitation training and progression tracking with the following features:
Alke Bracelet (Misfit) — A wearable that tracks range of motion, provides buzz notifications and detects emergencies.
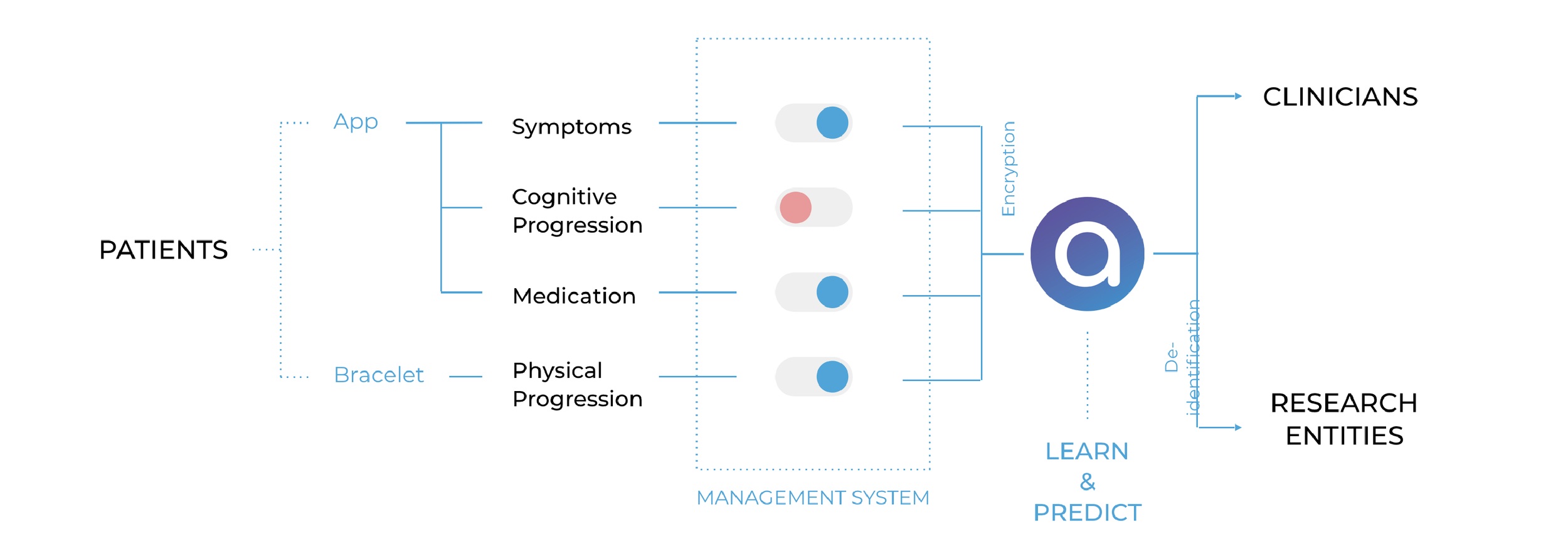
Alke’s System and Data flow
With Alke, by using the app, the bracelet and the box, patients can connect to their carers, clinicians, other patients and support organisations.
We give the patient the power to decide whether they want to share the data we collect, and to what extent they want to share.
Alke’s benefits and Business Model
Alke’s value proposition:
Alke’s benefits:
Alke’s business model:
Validation
We validated our service in three categories:
Desirability
Viability
Feasibility
Desirability
We had several different methods to test the desirability:
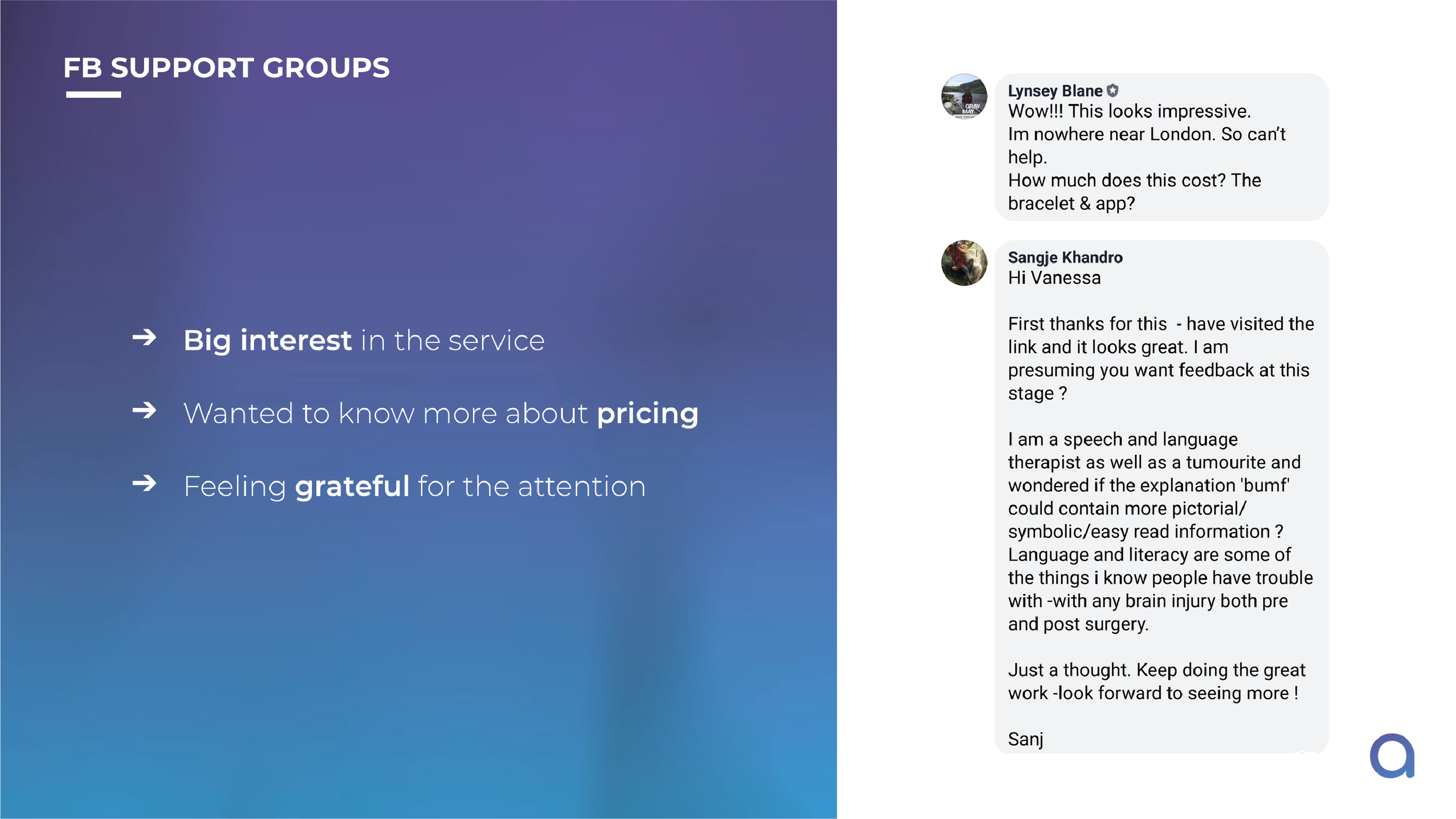
Website launch & Facebook group feedback: We designed a product launch website to understand the reactions of members of Brain Tumour support group members (patients and carers).
1:1 testing session: We visited carers and survivors to have a 1:1 feedback session about the service and the prototype.
Group testing session: We attend support group meeting to present the service, the box and the app. Afterwards, we had feedback sessions, both as a group and with individuals.
MVP prototype: We sent our Box to one of the survivors for a week. Instead of the app, we sent them text reminders about different tasks they can do. We also sent a GoPro camera for documentation.
Alke’s Website Launch and the feedback (www.alkeapp.com)
1:1 Testing session
Support group testing session
MVP Prototype Testing
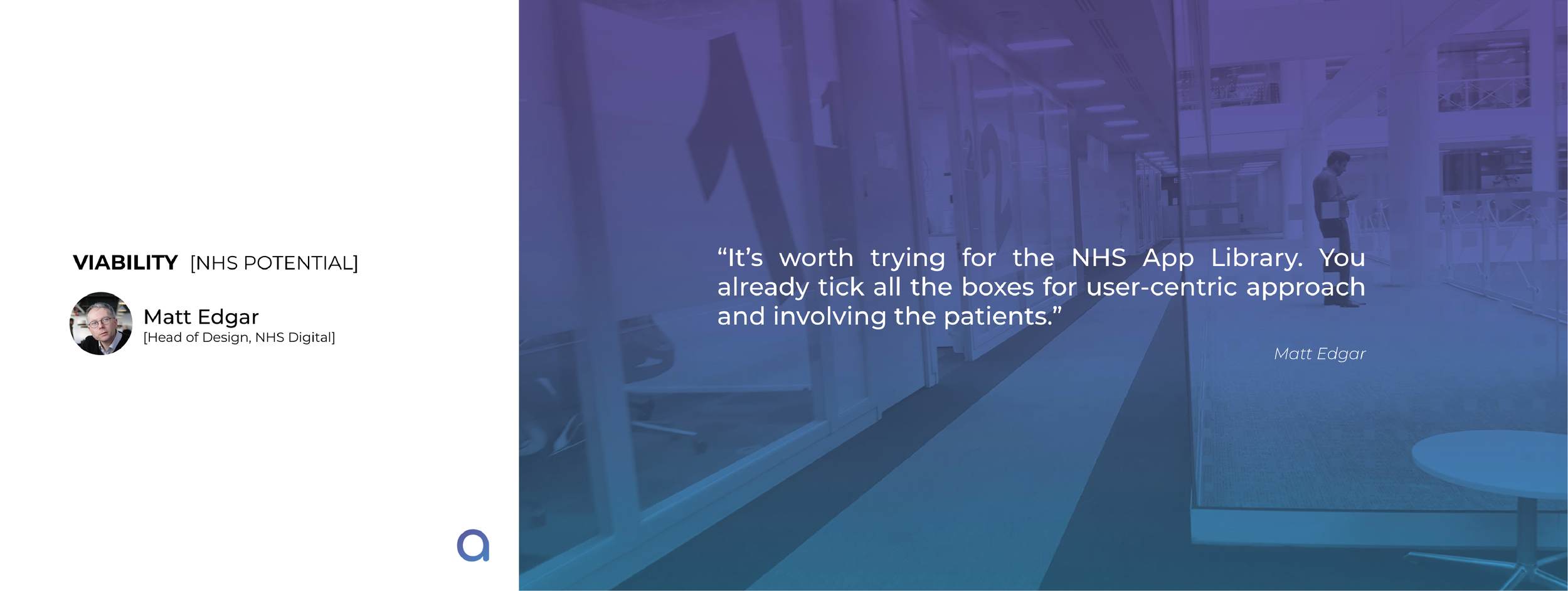
Viability
To test the viability, we met with 2 doctors working at the Health Foundry who mentor start-ups in healthcare innovation, as well as speaking to head of design at NHS Digital.
Feasibility
For feasibility, we talked to different engineers from the robotics industry.
Impact
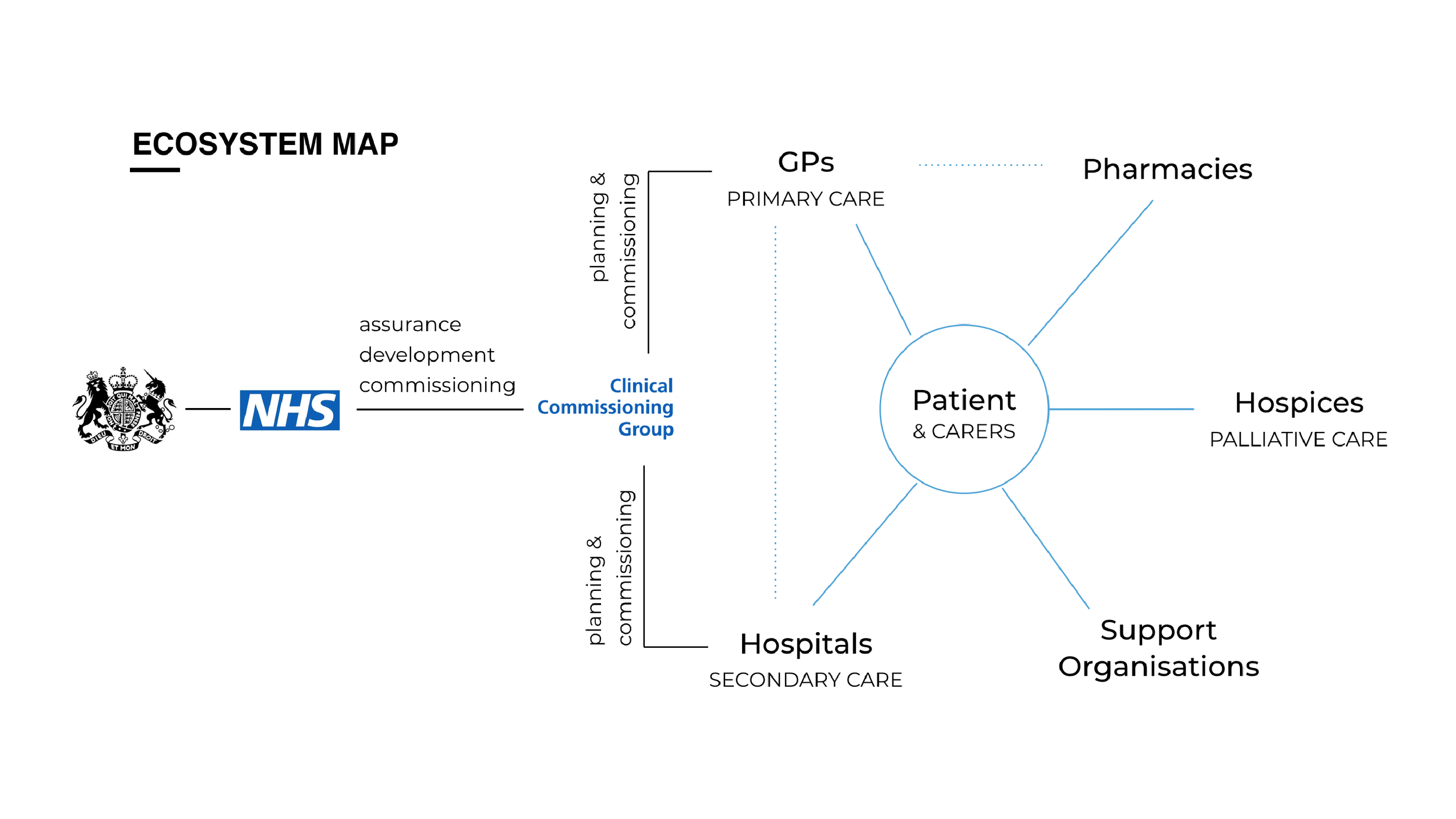
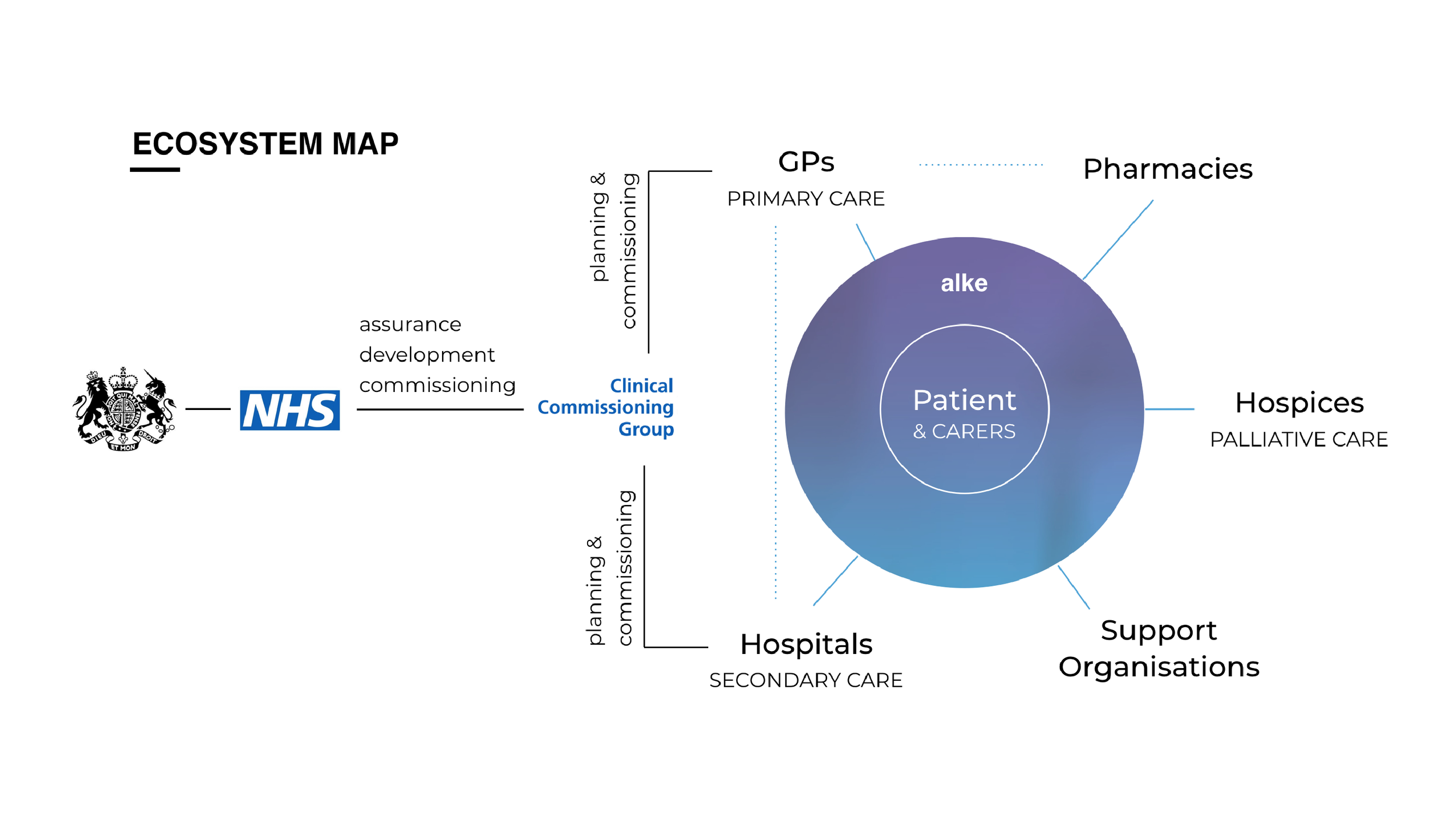
Going back to the initial ecosystem map, Alke acts as a bridge for the patients and carers in connecting them with different communities.
And for the emotional journey, we hope to transform the graph by elevating the various pain points throughout the journey.
How I got here
The process methodology used was the Design Council’s double diamond, with particular focus on having a user-centric empathetic approach. Using this approach meant that no assumptions were made at the start about the nature of the problems, and thus all our insights were based on the exact needs and challenges communicated to us by the users, the people with brain tumour and their carers. We sought to develop an inclusive and empowering way of creating change to improve the lives of all those involved.
01. Discover
The purpose of this stage was to understand the current system, as well as to engage with the primary stakeholders understanding their pains.
We conducted numerous interviews, travelling around UK (London, Basildon, Birmingham, Worcester, Walsall, Derby) in order to meet with patients, carers and clinicians. As a result, we met with 3 clinicians, 4 patients including 1 terminal patient, 6 carers, as well as the Head of Support of the Brain Tumour Support charity.
During this stage we used exploration activities, such as journey mapping as our primary tool. We wanted to listen and experience the whole journey from the patients’ and the carers’ perspective in order to highlight not only the functional bits of the process, but also their emotional rollercoasters. This helped us tremendously in understanding the timeframe of battling the tumour, as well as what their life was like before the tumour and how it has changed after the tumour.
Most importantly, we learned about how they were coping with their current issues, in addition to the systems and techniques they had to develop themselves in order to overcome the challenges. For example:
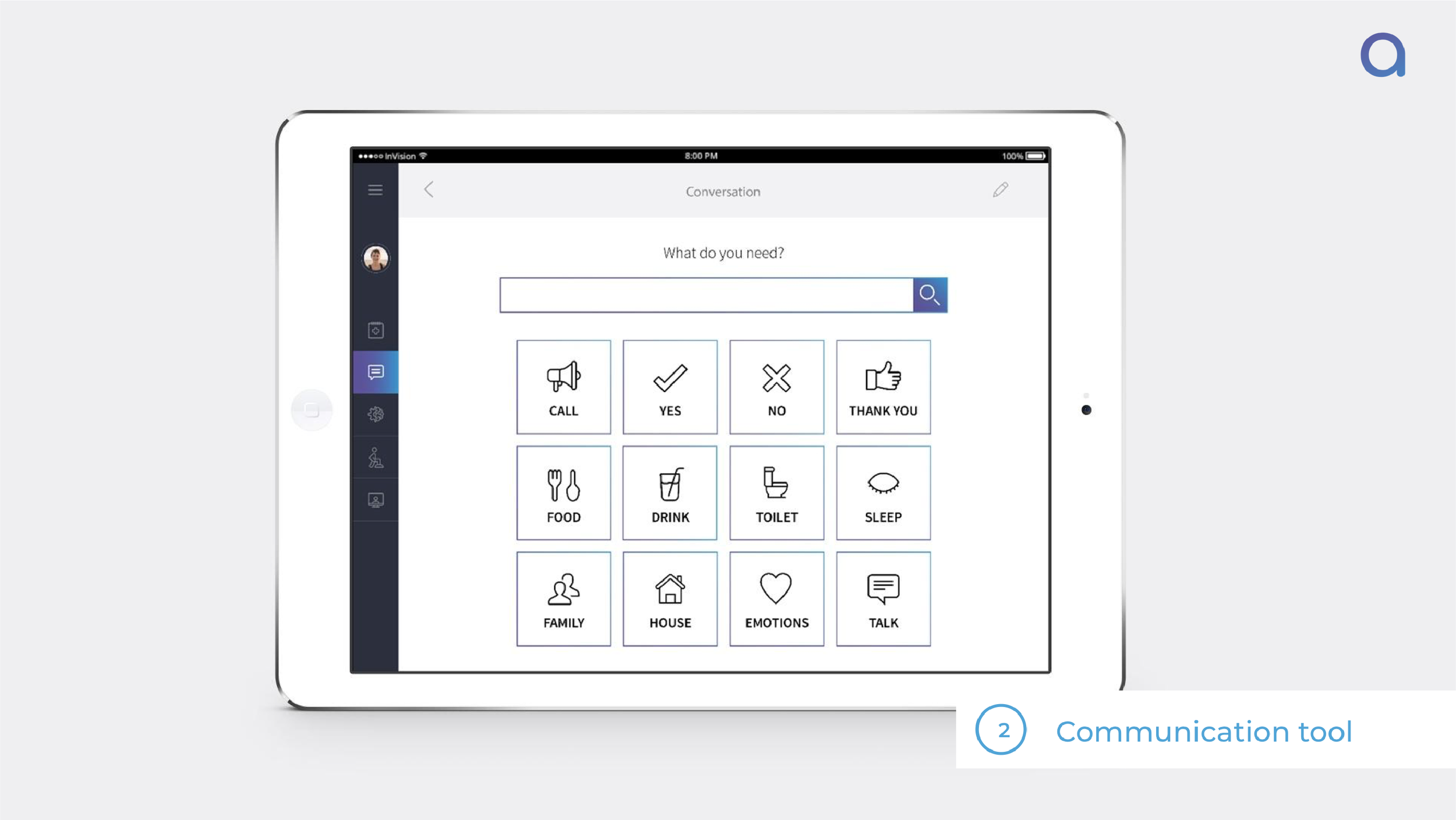
One of the carers, whose late wife had difficulty with mobility and suffered from expressive aphasia (difficulty finding the words to express their thoughts), had to develop a technique himself in order to better communicate with her. They had their own system, where his wife would bang her stick twice on the floor if she wanted him to come upstairs.
Another patient had noticed that often times, the 10-minute consultations were short, rushed, and overwhelmed him with information about which he had no time to look back and ask questions. So he started a diary, taking notes about his symptoms, doubts, curiosities, and emotions whenever he felt like it was important, in order to share them with the consultants.
These insights became very valuable to us in creating touch points and service principles.
Along with primary sources, we followed blogs and read books written by the patients themselves as well as survivors and carers, and generated journey maps for these experiences as well. We were able to learn about the pains and emotions, and more accurately document all steps of the experience.
In addition to the activity-based interviews with the main stakeholders, we created an online survey and shared it on various social media support groups for brain tumour patients and carers. We received a total of 42 responses, 29 from patients and 13 carers. The survey gave us a wide-ranging quantitative understanding of the issues they are facing and verified the insights we had already obtained through in-depth interviews.
02. Define
The purpose of this stage was to synthesise all the information obtained from the previous stage in order to establish the variables and the problem statement, as well as to set the objectives and principles for the service. To achieve this, we laid out all of our findings and started the affinity clustering. Through the clustering, we were able to distinguish themes and patterns that helped us define six variables:
Control: Patients and carers feel like they’re losing control and that the tumour is driving their lives.
Communication: Communication between patients and carers, as well as with clinicians, is difficult and inefficient.
Trust: Patients and carers do not fully trust the clinicians and the system.
Convenience: Patients need a simple, concise and easy way to access service.
Dignity: Patients are losing confidence and dignity through their battle with the tumour .
Emotion: Patients and carers go through an emotional roller-coaster during the journey due to a lack of support and information.
With these six variables, we were able to establish our two problem statements for the patients and their carers:
How might we create a personalised support service for patients with a brain tumour by leveraging technology to help them regain control of their lives, increase independence and reduce hospital visits?
How might we support carers in balancing their caring roles and maintaining their desired quality of life by ensuring that they receive both the medical knowledge and emotional support needed to manage the patient’s conditions?
The objectives of our service not only reflect these six variables but also shape our principles:
During this stage, we also mapped out our stakeholders by diagramming the network of people involved in the system, both directly and indirectly involved. Documenting the stakeholders allowed us to focus on the people and set a clear vision for the users.
3. Develop
The purpose of this stage was to develop our service proposition. With our objectives and principles identified, we began brainstorming, following ideation techniques to design touchpoints. In order to achieve this, we mapped out the user journey, highlighted the pain points in each stage and correlated them with our ideas. In parallel, we created personas for the patient, the carer and the clinician, which not only summarised our findings but also reinforced the empathetic element that challenged ourselves for our concept development.
Once we completed our concept ideation, we documented all of our touchpoints on a blueprint. This allowed us to think through every detail of each touchpoint of our service proposition by raising questions such as: what is the physical evidence? What needs to be completed in the back-end to move on to next stage? What data is collected at this point?
As a result, we developed Alke. Alke comes from the spirit and personification of courage and battle-strength in Greek mythology. It is a service for people with a brain tumour and their carers, which helps them understand, adapt and easily manage their rehabilitation on a daily basis.
Alke has 3 main components that play together in one holistic journey:
➔ Alke Box, containing:
Instruction cards, to inform patients and carers about the objects
Alke bracelet
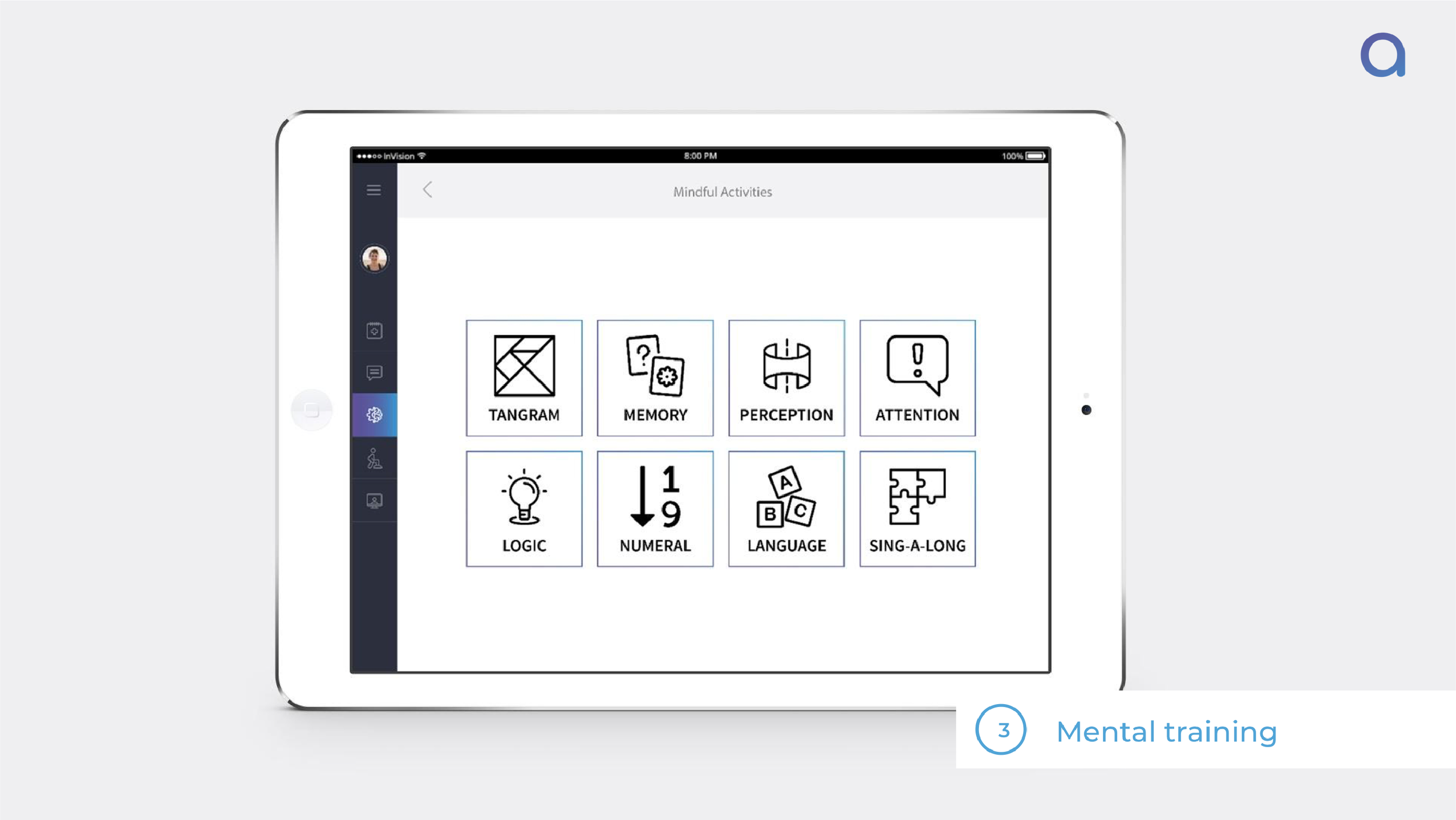
Mental activity game — for cognitive training.
Squeezy ball — for strength training and stress relief.
Hobby supplies — an element to bring the patient’s pre-tumour life back.
➔ Alke App, with the following functionality:
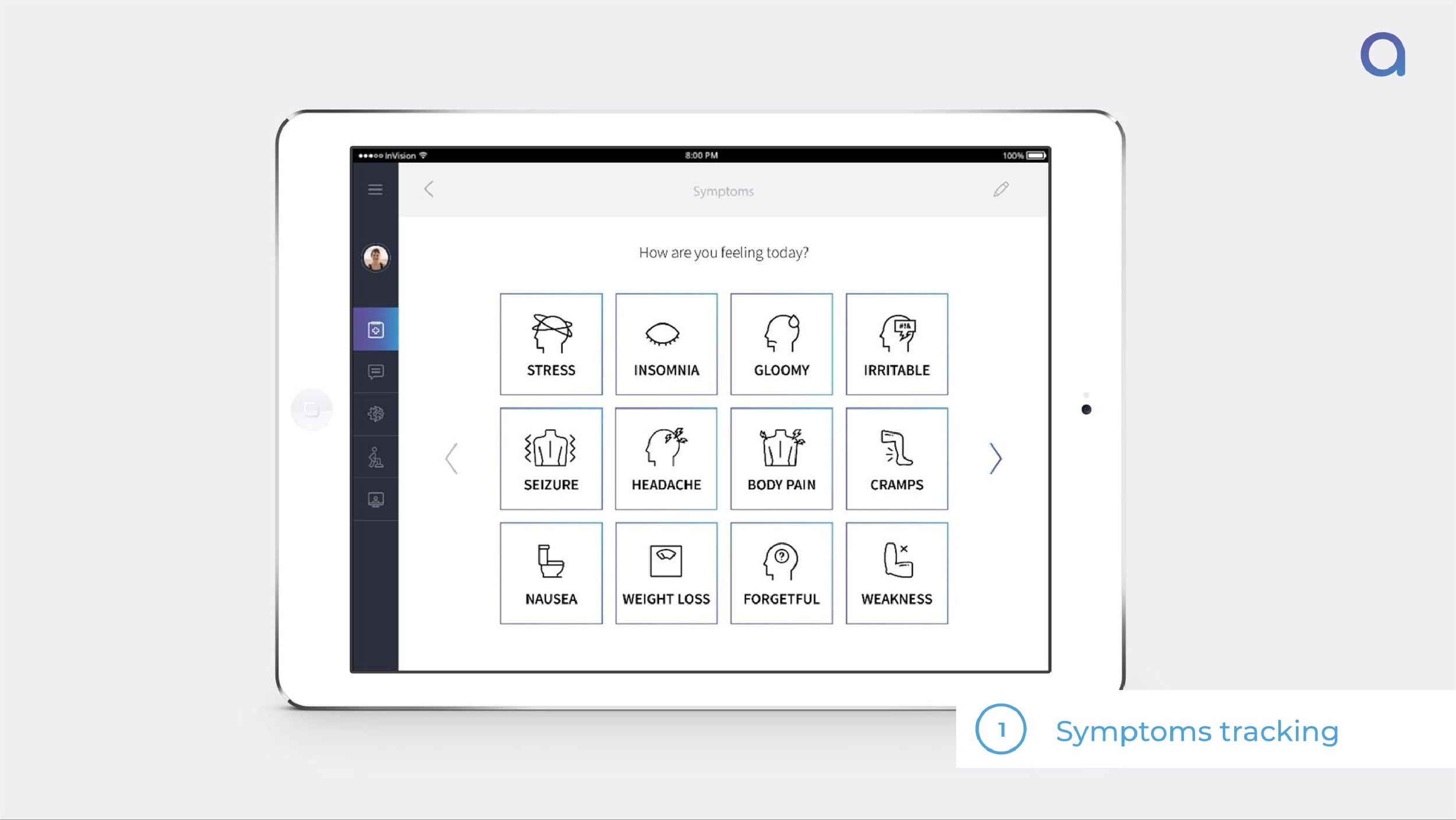
Symptom tracker — A diary where patients and carers can log their emotions and symptoms and state their intensity, which they can later share with their consultants if desired.
Communication tool — For patients with speech difficulties to easily communicate their needs and emotions.
Physical activities — To rebuild damaged muscles and strengthen neurophysical functions.
Cognitive activities — To stimulate and strengthen mental functions.
Teleconsultation — To allow patients and carers to prepare for the consultations keeping notes and questions and have online video consultations with clinicians.
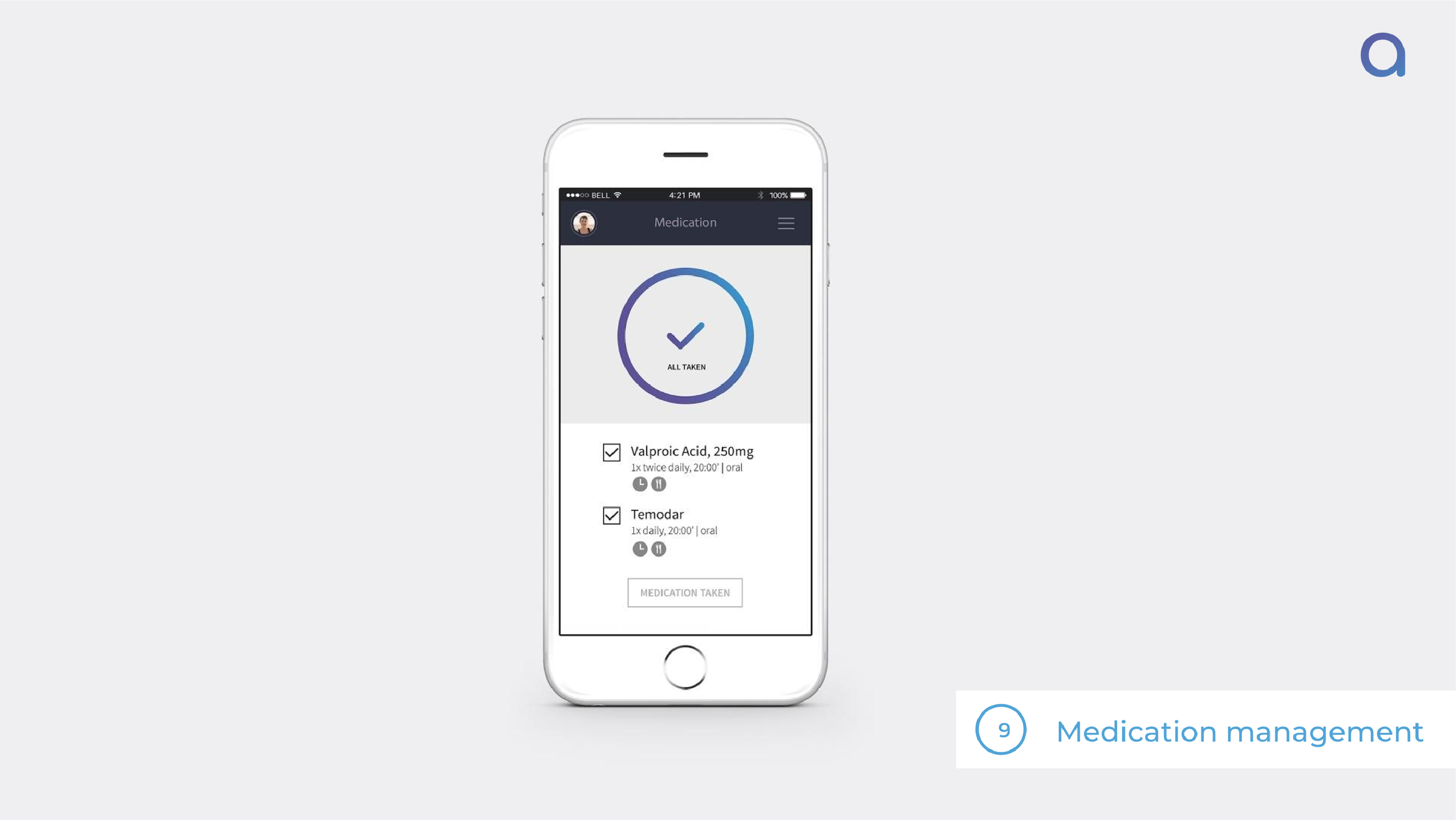
Medication management — To send alerts, reminders and display real-time pill intake status.
Alke to Alke — For patients to connect with other patients with similar journeys from around the world.
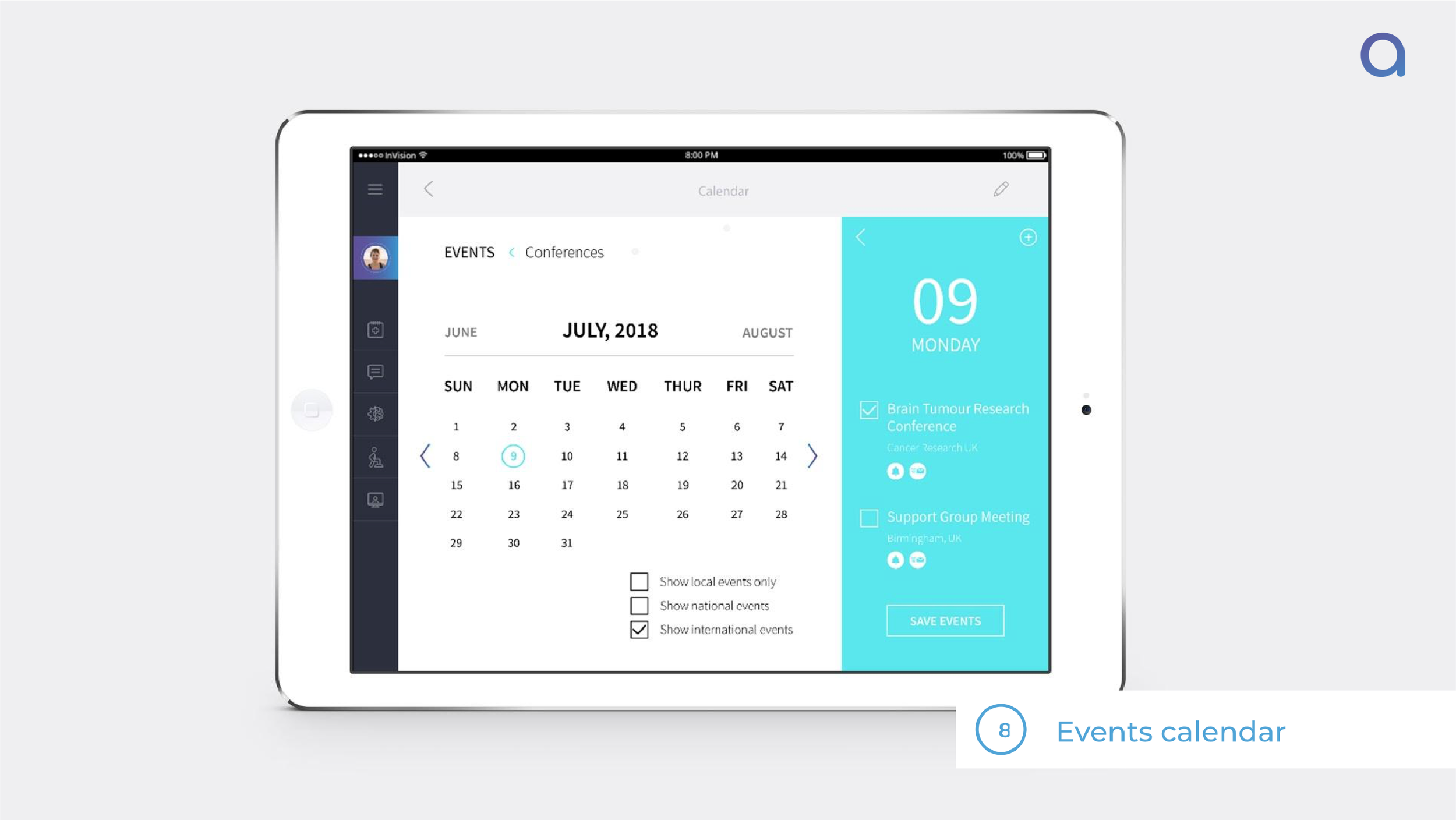
Events Calendar — With information from support groups and charities on upcoming events, conferences and support group meet-ups.
➔ Alke Bracelet, which:
Tracks physical activities patients are performing
Alerts for medication intake
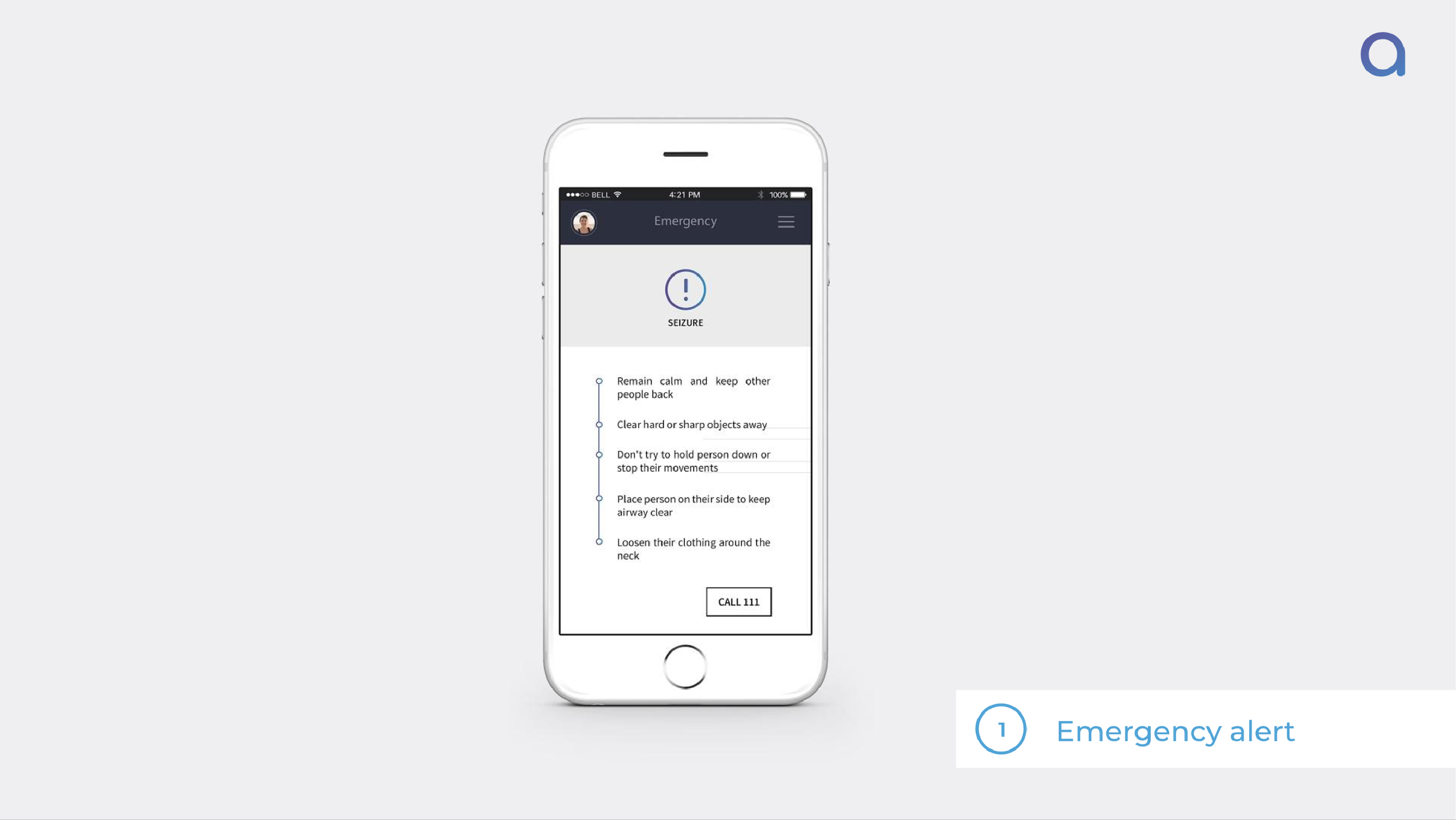
Detects seizures and falls and notifies carer
Monitors heartbeat
These three components along with a back-end of data analysis, kit personalisation, technical support and customer support, as well as a support network including rehabilitation experts, other patients and support charities, aligns with the established objectives and thus improves the rehabilitation journey for both patients and carers.
4. Delivery
We then combined what we learned and documented in the blueprint and personas to create a storyboard. For the storyboard, unlike the blueprint, we wanted to show the journey from a patient-and carer-centred point-of-view. We wanted to illustrate how Alke works, and how it improves the quality of the user’s rehabilitation journey. We then looked into content development of the box and the app.
We created physical and digital prototypes of the Alke Box and Alke App, in order to reach out to people for testing and validation of the service. We validated our service within three categories, Desirability, Feasibility, Viability, conducting different experiments and following different methodologies.
For Desirability, we tested the attractiveness of the service to the core users, as well as its usability and usefulness, by conducting 1:1 interviews with carers and patients in which they were able to use a working prototype of Alke app and interact with the Alke box. We also organised a feedback forum during a Brain Tumour Support group session in Birmingham in which we introduced the service, in addition to posting Alke’s website on various social media support groups to receive feedback from patients with a brain tumour and their carers.
Furthermore, in order to acquire more targeted feedback on our physical prototype of the kit and its use, we sent the Alke Box to a patient for 10 days, asking them to interact with it and document their experience. This patient’s persona aligned well with the persona according to which the prototype was designed for.
In terms of Viability, we explored the potential of the service being implemented in the real world by sharing our service proposition with Dr Neha Tanna & Dr James Somauroo, experts from the Health Foundry (an incubator for digital health innovation unit), in order to understand how Alke could play a role in the healthcare business world. We also shared our service proposition with the Head of Design at NHS Digital, Matt Edgar, to understand how Alke could fit in to the public healthcare sector.
Finally, in terms of Feasibility, we explored how the technology for the service might be developed by interviewing three technology experts (Mechanical Engineer, Electrical Engineer, Engineering Technologist in Automation & Robotics) so as to understand the scope of the technology used in Alke and its potential.